written by Carmen Phillips
A new study has revealed some important information about the behavior of one of the most notorious types of cancer. Studies have found that when pancreatic cancers run out of the sugar molecule glucose, which is their main source, they easily turn to alternative energy sources to survive.
Pancreatic tumors typically form a dense focal structure around them, an area often referred to as the tumor microenvironment. It also often lacks intact blood vessels. This unruly structure surrounding these tumors creates conditions that reduce the supply of glucose, an essential fuel source for normal and cancer cells.
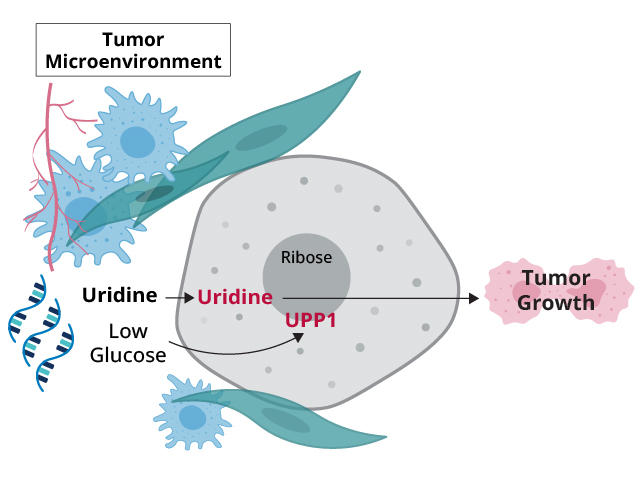
In this study, partially funded by NCI, an international research team showed that pancreatic cancer cells appear to have a powerful strategy to overcome this glucose deprivation: Pancreatic cancer cells It uses a molecule called uridine, which is an alternative fuel source.
Experiments using human pancreatic cancer cells grown in laboratory dishes showed that uridine becomes the cells’ main energy source when glucose is insufficient. And when pancreatic cancer cells that cannot use uridine were transplanted into mice, only small tumors formed, according to research published on May 17th. Nature.
Related research published on the same day natural metabolism, this result provided strong support. In that study, researchers reported that other types of cancer cells may also rely on uridine for energy when glucose is unavailable.
More research is needed to see if there is a way to use this information to develop new treatments for pancreatic cancer, one of the researchers admits. Nature Dr. Kostas Lysiotis of the University of Michigan Medical School, the study’s principal investigator.
Dr. Lysiotis explained that blocking the way cancer cells obtain and use energy, or their metabolism, is difficult as a treatment. But a better understanding of how cancer cells adapt metabolically to the often oxygen- and nutrient-starved environments in which they exist is opening up other avenues for attacking cancer cells. He said it could be opened.
Identifying alternative energy sources for cancer cells
Pancreatic cancer is one of the leading causes of cancer death. Its harsh microenvironment not only thwarts the entry of drugs designed to kill tumors, but also allows other residents within and around tumors to create an ecosystem that helps tumors grow. research shows.
However, this microenvironment also has downsides for tumors. This means less oxygen can flow into the tumor. Dr. Lysiotis said pancreatic tumors in particular are “highly avascular.” And not only are blood vessels often missing, but even when they do form, they often leak or break.
This abnormal vascular structure can limit the nutrients available to the tumor and cause “glucose starvation,” said Dr. Konstantin Salnikov of NCI’s Division of Cancer Biology.
Other studies have shown that pancreatic tumors can obtain energy from sources other than glucose. But Dr. Lysiotis’ research team, along with colleagues at the Institute of Cancer Research in London, wanted to dig deeper and identify the specific nutrients that pancreatic tumor cells take up to support their energy needs.
Uridine: Not a typical fuel for cancer cells
The research team began by using an advanced testing platform specifically designed to analyze nutrients in blood and other tissues. Researchers used this tool to test 175 types of cancer cells by about 20 different human pancreatic cancer cell lines (pancreatic cancer cells kept alive in a laboratory dish) when glucose was not available. We evaluated how easily the above nutrients could be taken up.
The analysis identified many of the “common suspects” that cancer cells would expect to use as fuel, Dr. Lysiotis explained. But uridine stood out.
First, because uridine is a structural component of RNA, it is different from typical energy sources that cells rely on, such as carbohydrates such as glucose, Dr. Lysiotis said. It was also readily used in all pancreatic cancer cell lines tested.
Additionally, they found a strong association between high activity of a gene called . UPP1 and the use of uridine by pancreatic cancer cells. The latter finding is an important piece of the puzzle, Dr. Lysiotis explained.
Like the sidecar of a motorcycle, a sugar molecule called ribose is attached to uridine. Ribose is also a component of ATP, the main energy carrier in cells. UPP1 is a protein produced when: UPP1 It is active and interacts with uridine in cells to release ribose, which cells can use to meet their energy needs.
Analysis of tumor samples from pancreatic cancer patients revealed an association between high levels of UPP1 and shorter survival. Other experiments on cancer cell lines also strongly suggested that UPP1 strips ribose from uridine, which cells use for energy.
Analysis of mice with pancreatic tumors confirmed what the researchers observed in cell line experiments. When mice were injected with pancreatic cancer cells that lacked function, UPP1 Tumors containing the UPP1 gene (meaning the cells cannot produce the UPP1 protein) were much smaller and progressed more slowly than tumors formed from cells with the complete form of the gene.
“We were very surprised by how strong an effect” the absence of UPP1 had on tumor growth, Dr. Lysiotis said.
Where do cancer cells get uridine? RNA!
Survey results from natural metabolism The study, funded by the NCI and conducted by researchers at Harvard University, the Massachusetts Institute of Technology, and the University of Lausanne in Switzerland, is largely consistent with their own work. Nature study.
The study showed that some cancer cells, including skin and brain cancers, phagocytose uridine to meet their energy needs when glucose is not available. Other cell types, including immune cells, responded similarly. The researchers also reported: UPP1 (and related genes, UPP2) was highly active in cells when glucose was limited.
But the key question for both research teams was: Where did the cells acquire uridine? Dr. Lysiotis’ team’s analysis pointed to multiple sources in and around the tumor, including immune cells called macrophages. However, related studies directly pointed to RNA.
In fact, when cancer cells lacking glucose were given large amounts of RNA, they proliferated just as well as when glucose was present.
“I remember telling my friend that we had done this crazy experiment where we fed cells with RNA,” one of the study co-leads, Dr. Alexis Jardin of the University of Lausanne, said in a news release. “I didn’t think this would work. I was very surprised to see the cells grow.”
Dr. Lysiotis agreed that RNA is likely the primary source of uridine in cancer cells when glucose is limited.
The fact that cancer cells obtain uridine from RNA “has important implications for cancer biology,” Dr. Salnikov said. “RNA is a very abundant molecule,” he continued. Therefore, all types of tumor cells may rely on RNA to drive their metabolism.
It’s also possible that RNA may not be the only source of uridine in glucose-starved cancer cells, says Dr. Perlmutter, a radiation oncologist at New York University Langone’s Perlmutter Cancer Center who focuses on cancer cell metabolism. said study author Michael Pacold, MD.
“There are probably multiple sources,” Dr. Pacold says. Tumors are “incredibly adaptable” when it comes to getting the energy they need, he continued.
Targeting metabolism as a cancer treatment
Since there are few effective treatments for pancreatic cancer, the obvious question is whether any of these findings suggest new treatments, Dr. Lysiotis said.
Although great progress has been made in understanding cancer cell metabolism, much work still needs to be done to find ways to harness it for potential treatments, he explained. Pancreatic cancer is particularly difficult.
Pancreatic cancer cells are “professional scavengers,” he says. “If you shut off one fuel source, they’ll find another.”
According to Dr. Pacold, many of the most effective chemotherapy drugs that have been used for many years work by interfering with cellular metabolism (often called antimetabolites), so they target specific aspects of cancer cell metabolism. There is already strong precedent for this.
In fact, many experimental drugs that interfere with metabolism in different ways are being tested in clinical trials.
Dr. Pacold said he hopes that “identifying additional metabolic dependencies will help improve cancer treatment.”