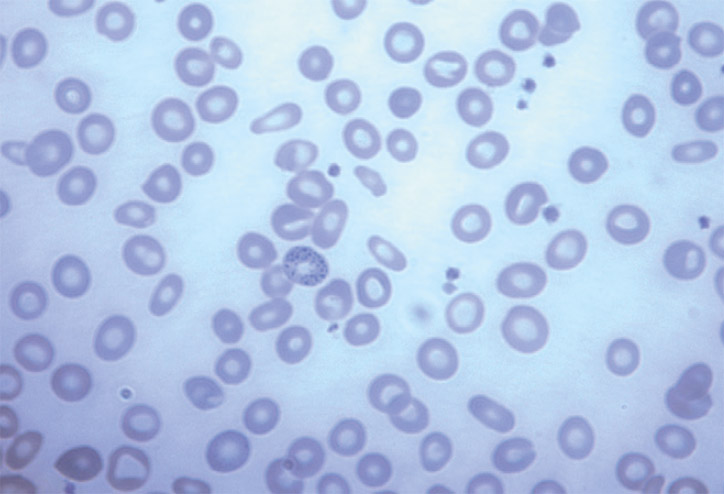
Figure 1. Blood film showing basophilic stipples.
What is the role of traditional medicine in Australia?
Ayurvedic medicine (AM) and Traditional Chinese Medicine (TCM) play an important role in Australian society, with at least two in three Australians reporting using complementary medicine within the past 12 months doing.1 Heavy metal toxicity is a known complication of AM and TCM but is often overlooked in medical evaluation. With an increasing number of Australians accessing medicines via the internet, primary care clinicians are now using traditional and herbal medicines regularly to treat heavy metal poisoning in patients presenting with unexplained anemia and abdominal symptoms. We must remain vigilant. Identification of the source of exposure is essential to the management of heavy metal poisoning.
Heavy metal poisoning in traditional medicine: is it a problem?
Herbal products used in AM and TCM are increasingly scrutinized for heavy metal content. In 2005, Australia’s Therapeutic Goods Administration (TGA) issued a safety alert regarding heavy metal toxicity from AM.2 While it is reassuring that Australian herbal manufacturers must be licensed by the TGA, it is important to note that TGA oversight does not extend to imported products for personal use. Consumers may not be aware of the potentially high heavy metal content in imported herbal medicines or the negative effects of heavy metal intake. Complications from heavy metal toxicity often exacerbate the underlying disease of heavy metal administration, resulting in increased morbidity for patients.
Of the cases regularly reported around the world, lead poisoning appears to be the most common heavy metal poisoning. Arsenic poisoning, including skin symptoms and hemolytic anemia, has been reported with oral and topical use of AM and TCM.3~6 Toxic levels of other heavy metals such as cadmium and mercury have also been reported to be present in herbal preparations. One study found that more than a fifth of the Ayurvedic products he bought online contained detectable levels of lead that exceeded acceptable intake standards.7
What is lead poisoning and how does it manifest?
Because lead toxicity is a rare condition, diagnosis poses several challenges and requires a high degree of clinical suspicion. Diagnosis is assisted by a complete blood count and blood film showing classic basophilic stippling and confirmed by elevated BLL (>0.48 μmol/L or 10 μg/dL). The clinician’s first job is to identify and eliminate the source of lead exposure. Previously, common sources of lead included lead-containing paint and gasoline. Occupational and industrial sources remain potential sources in modern times, as well as fishing sinkers and lead-contaminated soil in children with pica. In recent years, herbal medicines such as AM and TCM have been included as sources of heavy metal toxicity.8~12
Lead poisoning often manifests as non-specific signs and symptoms and affects multiple systems. Obvious clinical toxicity from lead may not become apparent until BLL exceeds 40 µg/dL.13, 14 However, subclinical toxicity in adults with hypertension and renal impairment is known to occur at lead levels below this threshold. The most common symptoms are abdominal pain, constipation, fatigue, and decreased cognitive function. More severe toxicities include encephalopathy and seizures. Children are particularly susceptible to the effects of lead, and low lead levels can cause intellectual disability and neurodevelopmental disorders.14,15 Therefore, the American Academy of Pediatrics (AAP) and the Centers for Disease Control and Prevention (CDC) recently lowered the monitoring threshold for lead to 5 µg/dL.16
How is lead poisoning managed?
Managing lead toxicity includes identifying and removing the source of lead, notifying the appropriate authorities, and possibly reducing the burden of lead in the body through chelation therapy. DMSA, the oral chelator of choice, may be indicated in symptomatic patients with elevated BLL.13 Various guidelines recommend BLL threshold treatment for asymptomatic patients. The duration of treatment is usually 2-3 weeks but depends on the trend of BLL and improvement of clinical symptoms. Common side effects of DMSA therapy include gastrointestinal disturbances, skin rash, elevated liver transaminases, fever, and neutropenia.17 Trace element deficiencies can occur with all types of chelation therapy, especially the removal of iron, zinc, and copper. In cases of severe toxicity causing lead encephalopathy, patients may require hospitalization and intravenous chelation therapy. In most cases of lead poisoning, expert advice from the Australian Poisons Information Center (13 11 26) or a clinical toxicologist is recommended.
Key Point
- Many Ayurvedic and traditional Chinese medicines contain large amounts of heavy metals (particularly lead, arsenic, and mercury), far above recommended limits.
- Regular use of Ayurvedic and traditional herbal medicines can lead to heavy metal poisoning. A thorough medical history should be taken, including the use of traditional medicines.
- Blood films showing basophilic puncta remain an important diagnostic tool for lead toxicity.
Competitive relationship: None.
Provenance and peer review: Not commissioned. Has undergone external peer review.
