Our study found that vitamin A is associated with a lower risk of diabetic retinopathy. In particular, vitamin A was found to be more associated with a lower risk of diabetic retinopathy in men and young people under 60 years of age. It was also found that the risk of developing diabetic retinopathy was lower when the blood vitamin A concentration was more than 0.51 and less than 0.64. compared to other vitamin A concentrations in the blood. This study is the first to examine the relationship between serum vitamin A and the risk of diabetic retinopathy.
The reason for this result that vitamin A reduces the risk of diabetic retinopathy can be explained by the pathogenesis mechanism of diabetic retinopathy and the mechanism of action of vitamin A. The pathogenesis of diabetic retinopathy includes angiogenesis, inflammatory response, and fibrosis.14,15. Due to these etiologies,, Diabetic retinopathy develops complications such as non-proliferative diabetic retinopathy, proliferative diabetic retinopathy, vitreous hemorrhage, and traction retinopathy.16,17. Conversely, vitamin A has anti-angiogenic, anti-inflammatory response, and anti-fibrotic functions that are counter to the development of diabetic retinopathy.18,19. Vitamin A is a potent regulator of cell differentiation and proliferation and acts as an immunomodulatory and antiangiogenic agent.20, 21, 22. Vitamin A is one of the representative antioxidants and has anti-inflammatory effects, protecting the body from inflammation in the body by removing active oxygen in the body and improving immune function.23,24. Because vitamin A has antifibrotic effects, research is being conducted into the treatment of vitamin A-binding drugs in diseases such as pulmonary fibrosis, liver fibrosis, and skin fibrosis. Vitamin A is also expected to have an anti-fibrotic effect on the retina of the eye.25, 26, 27, 28. These reasons explain why vitamin A reduces the risk of diabetic retinopathy.
This study found that vitamin A was associated with a lower risk of diabetic retinopathy, especially in men. These results can be explained by biological, social behavioral, and cultural differences between men and women. One study found that the average levels of each biomarker varied significantly by sex at birth, with cardiometabolic biomarkers higher in men and inflammatory and neuroendocrine biomarkers higher in women. However, over time, gender biomarker characteristics were mediated, attenuated, or interacted in response to differences in social environment.29.
Our study found that higher blood vitamin A levels were associated with a lower risk of diabetic retinopathy, especially in people under 60 years of age compared to people over 60 years of age.. Vitamin A acts in the visual system by converting between all-trans retinal and 11-cis retinal.30. In older people, metabolic activity in the body decreases with age. This may explain why blood vitamin A levels have a greater effect on lowering the risk of diabetic retinopathy in young people under the age of 60. It is thought that mitochondrial function declines with age, making the retina less sensitive to vitamin A, resulting in these results.31,32. The effects of vitamin A may be greater in younger people because their photoreceptors are more metabolically active.
Level 3 of vitamin A was more effective than level 4 in reducing the risk of diabetic retinopathy. It was also found that blood vitamin A levels between 0.51 and 0.64 were associated with a lower risk of developing diabetic retinopathy compared to other vitamin A levels. Concentration in blood. Considering that the cut point for vitamin A is 0.64, vitamin A levels above 0.64 are less effective in reducing the risk of diabetic retinopathy than level 3. The normal range for vitamin A is 0.3 to 0.6. The normal upper limit for vitamin A concentration in the blood is 0.6. Therefore, excessive intake of vitamin A above normal limits is less effective in reducing risk. Although the exact reason is unknown, vitamin A is fat-soluble, so excessive intake of vitamin A is not good for diabetic retinopathy.
There are several studies on vitamin A and diabetic retinopathy. Ruamviboonsuk et al. reported that diabetic participants without retinopathy had lower serum vitamin A levels than the DR group. Serum vitamin A levels in DR patients were significantly lower than controls (P = 0.01). High serum vitamin A levels reduced the risk of developing DR by 31.1% (P = 0.007)33. Rostamkhani et al. reported that a decrease in blood vitamin A concentration was associated with the severity of diabetic retinopathy, followed by a group without diabetic retinopathy, a group with non-proliferative diabetic retinopathy, and a group with proliferative diabetic retinopathy. This was followed by the group with symptoms.12. Zhang et al. The group with diabetic retinopathy reported lower dietary vitamin A intake than the group without diabetic retinopathy.34. In the past, we conducted a survey on dietary vitamin A levels and the risk of diabetic retinopathy among 1,948 Korean adults aged 40 and older.13. However, we found no evidence that high levels of dietary vitamin A were associated with a lower risk of diabetic retinopathy. Our previous study did not find evidence of an association between vitamin A and diabetic retinopathy with dietary information. This does not mean that diabetic retinopathy is unrelated to dietary vitamin A, but it does mean that measuring the amount of dietary vitamin A has limitations. Vitamin A is a fat-soluble vitamin, and the rate of absorption may be altered if you have conditions such as small intestinal disorders, chronic malabsorption, or decreased pancreatic function.35. In addition, vitamin A ingested through food is absorbed into the blood and actually acts on the retina in various ways.30. Therefore, to assess the relationship between diabetic retinopathy and vitamin A, it may be better to measure vitamin A levels by blood type than by dietary type. This means that identifying associations through blood sampling can be more accurately and effectively confirmed and interpreted. result. Through this study, we found that higher blood levels of vitamin A are associated with a lower risk of diabetic retinopathy.
Diabetic patients with diabetic retinopathy require health policy and health education supplements. As diabetic retinopathy worsens, quality of life decreases, vision deteriorates, potentially dangerous accidents, and medical costs increase.36. Therefore, diabetic retinopathy patients require health policies or health education supplements for diabetes management and dietary management. Ultimately, education on dietary management to increase vitamin A, as revealed in this study, will be necessary. Through health policy and health education, we must ensure that patients have access to vitamin A and create an environment in which vitamin A can be synthesized successfully.
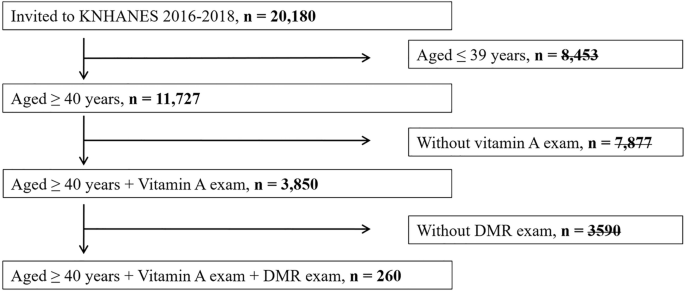
The strength of this study is that it was conducted on a large number of people through statistical multilevel cluster random sampling. Considering the formula for calculating the P value, statistical significance increases when the effect is large or the sample size is large. Conversely, a small sample size may reduce statistical significance. He selected 260 subjects suitable for the study from a total of 11,727 subjects, and the results showed statistical significance. The fact that a statistically significant result was obtained in a small sample actually has much greater statistical significance. Previous studies were mostly case-control studies. There may be selection bias in this. Our study is a population-based study, which is important compared to previous studies. We conducted a study of people with diabetes and diabetic retinopathy in the entire population without any sampling procedures. Additionally, measuring vitamin A levels in the blood rather than in the diet provides more scientific and accurate results. Our study has several limitations. The results of this study are from South Korea and are not representative of other regions. Further research is needed as other ethnic groups and regions may have different results. Our study is a cross-sectional study. Microvascular complications such as diabetic retinopathy occur as a result of long-term metabolic control that occurs several years before the onset of diabetic retinopathy, as previously reported in Asian populations.37. Therefore, cross-sectional vitamin A levels may not be representative of vitamin levels in the body over several years. Cohort studies with large sample sizes are needed. Models that adjust only for recent blood glucose levels and blood pressure should be interpreted with caution. Because it was a cross-sectional study, we could see that there was a correlation, but it was difficult to confirm causal relationships, that is, information that came first. The use of prospective health survey data remains necessary. This result is interesting and motivates large-scale studies to confirm the observations. Therefore, further studies in the future are needed to compensate for these limitations.
In conclusion, high levels of vitamin A in the blood are associated with a lower risk of diabetic retinopathy. In particular, a more effective relationship is seen among men and young people under 60 years of age. Increasing vitamin A in the blood to reduce the incidence of diabetic retinopathy is thought to help prevent diabetic retinopathy. Therefore, in order to increase vitamin A, it is necessary to create an environment where the body can ingest vitamin A or synthesize vitamin A on its own. Further research is considered necessary for future care, medical policy, and health education for patients prone to diabetic retinopathy.