Baseline Features
The clinicopathological characteristics of the 333 patients and their association with mGNRI are shown in Table 1. The majority of the included patients were male (n = 300, 91.1%). Of the patients, 118 (35.4%) were aged 65 years or older. The median (IQR) age and follow-up time were determined to be 60 (52–69) years and 42.1 (21.0–67.8) months, respectively. Buccal mucosa (n = 107, 32.1%) and tongue (n = 130, 39.0%) were the two most common tumor subsites. In addition, 74 (22.2%), 44 (13.2%), 50 (15.0%), and 165 (49.5%) patients had stage I, II, III, and IV OCSCC, respectively. Adjuvant therapy was administered to almost half of the patients, specifically 124 (37.2%) received CRT and 45 (13.5%) received adjuvant radiation therapy (RT). The majority of patients (n = 272, 81.7%) had at least two of the outlined personal habits. Before undergoing surgery, six of 333 patients (1.8%) required a nasogastric tube due to significant malnutrition and reduced oral intake.
Association between clinicopathological characteristics and mGNRI
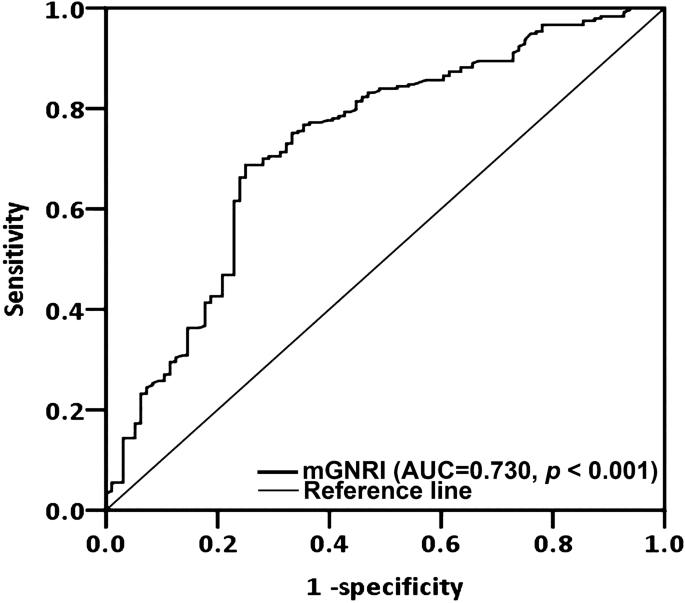
ROC curve analysis determined that the optimal mGNRI cutoff was 73.3 (AUC 0.730, specificity 75.0%, sensitivity 68.8%). p The AUC of mGNRI was higher than that of BMI (AUC, 0.611) and CRP (AUC, 0.712), suggesting that mGNRI has superior prognostic discrimination power compared with BMI and CRP. Therefore, the cutoff value of mGNRI was used to divide patients into low mGNRI group (< 73.3) (146 patients (43.8%)) and high mGNRI (≥ 73.3) group (187 patients (56.2%)). The clinicopathological characteristics of these groups are shown in Table 1. We found that mGNRI < 73.3 was significantly associated with the presence of ENE (p < 0.001), nearest resection margin < 5 mm (p = 0.046), stage III–IV disease (p < 0.001), need for adjuvant therapy (p < 0.001), DOI ≥ 10 mm (p < 0.001), and shorter median survival time (p < 0.001), and progressive T and N status (both p < 0.001). However, mGNRI was not significantly associated with age, sex, tumor subsite, personal habits, PNI status, LVI status, tumor grade, or CCI.
Cut-off values for mGNRI derived from receiver operating characteristic curve analysis. Commonwealth of Australia Area under the curve, GNRI Modified geriatric nutritional risk index.
Correlation between mGNRI and OS
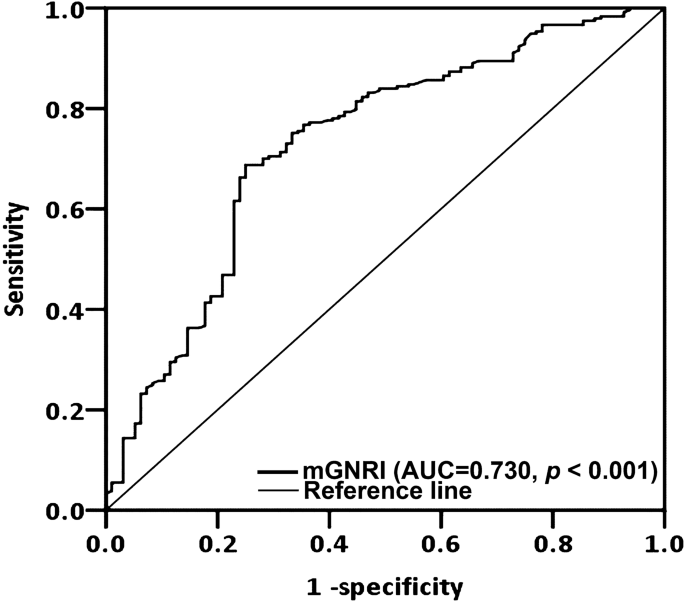
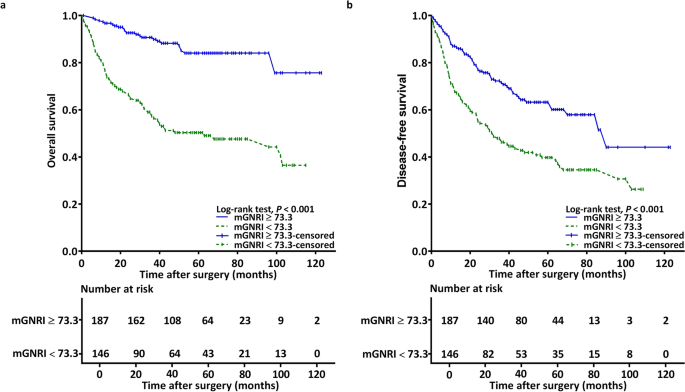
During the follow-up period, 96 (28.8%) patients died.Evaluating the plotted Kaplan–Meier curves, we found that the low and high mGNRI groups were significantly different in terms of 5-year OS rate (50.7% vs. 87.2%). p < 0.001 (Fig. 2a). Furthermore, samples were stratified by cancer stage, and the analysis revealed that a lower mGNRI was consistently associated with worse OS in both early-stage (Fig. 3a) and advanced-stage (Fig. 3c) cancers ( p The poor prognostic factor was mGNRI < 73.3 (HR 3.893, 95% CI 2.424-6.250). In univariate analysis, poor OS was significantly associated with mGNRI < 73.3, advanced stage disease, presence of PD, presence of LVI and PNI, CCI ≥ 1, and need for postoperative therapy (Table 2). In multivariate analysis, mGNRI < 73.3 was identified as an independent prognostic factor for poor OS (HR 3.893, 95% CI 2.424-6.250, p < 0.001). Other independent factors included stage III-IV disease (HR 2.052, 95% CI 1.159-3.635). p = 0.014), and the presence of PNI (HR 1.630, 95% CI 1.026–2.591). p = 0.039), PD (HR 2.453, 95% CI 1.476–4.077, p < 0.001), and LVI (HR 2.443, 95% CI 1.307–4.566). p= 0.005).
Kaplan-Meier curve (One) Overall survival and (b) Disease-free survival was categorized by preoperative mGNRI. An mGNRI value of less than 73.3 was significantly associated with poor prognosis. GNRIModified geriatric nutritional risk index.
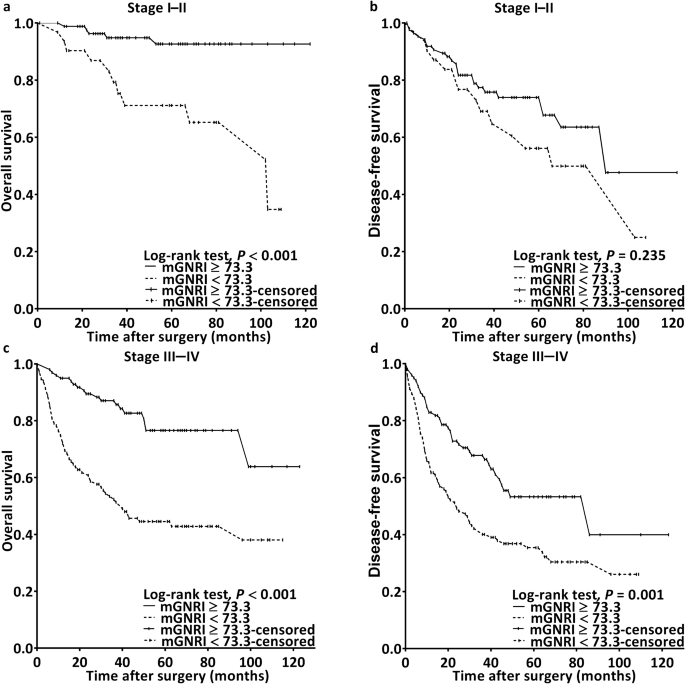
Kaplan-Meier survival curves for samples stratified by mGNRI and cancer stage revealed that patients with mGNRI < 73.3 were correlated with poor overall survival (One) Stage I-II and (c) Stage III-IV (both pSimilar results were obtained for disease-free survival in patients with BRCA1 (<0.001) disease.d) significantly improved in stage III-IV patients (p = 0.001), butb) Stage I-II disease (p= 0.235). GNRIModified geriatric nutritional risk index.
Association between mGNRI and DFS
Evaluating the plotted Kaplan–Meier curves, we found that the low and high mGNRI groups were significantly different in terms of 5-year DFS (39.7% vs. 66.3%). p< 0.001; Figure 2B). Furthermore, samples were stratified by cancer stage, and the results showed that low mGNRI was significantly associated with worse DFS in advanced-stage cancer (p= 0.001; Fig. 3D), but in the early stages (p= 0.235; Figure 3B). Univariate analysis showed a significant association between poor DFS and LVI status, tumor grade, need for adjuvant therapy, stage III-IV disease, and mGNRI < 73.3 (Table 3). Multivariate analysis showed that mGNRI < 73.3 (HR 1.803, 95% CI 1.292-2.517, p< 0.001), PD (HR 2.011, 95% CI 1.302–3.108, p= 0.002), and end-stage disease (HR 1.734, 95% CI 1.186–2.535; p= 0.005) was identified as an independent predictor of unfavorable DFS.
Stratified analysis of OS prediction
The association between mGNRI and OS was consistently significant when patients were stratified by tumor subsite, age (≥65 or <65), N status (N0 or N1–N3), T status (T1–T2 or T3–T4), ENE status (absent or present), PNI status (absent or present), nearest surgical margin (≥5 mm or <5 mm), and DOI status (≥10 mm or <10 mm) (Figure 4).
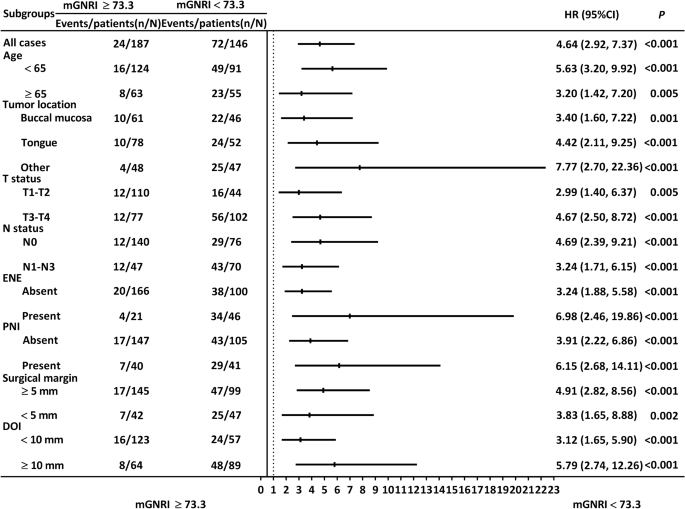
Stratified analysis investigating the association between mGNRI and OS. Consistent trends were observed in all subgroups. CIConfidence interval, Publication dateThe depth of the invasion East NortheastExtranodal extension, human resourcesHazard ratio, GNRIModified Geriatric Nutritional Risk Index, IndividualPerineural invasion.
OS prediction nomogram
The nomogram we constructed included the significant prognostic factors obtained from the multivariate analysis, namely, mGNRI, cancer stage, tumor grade, PNI, and LVI (Fig. 5a). The C-index value obtained with the mGNRI-based nomogram was 0.781 (95% CI 0.751–0.813), whereas the C-index value obtained with the AJCC stage-based nomogram was 0.631 (95% CI 0.605–0.658). To further verify the accuracy of the nomogram, we constructed calibration plots showing the probability of 3- and 5-year OS (Fig. 5b, c, respectively). Both calibration plots were closely aligned with the 45° diagonal line, implying that the calibration accuracy of the constructed nomogram is high.
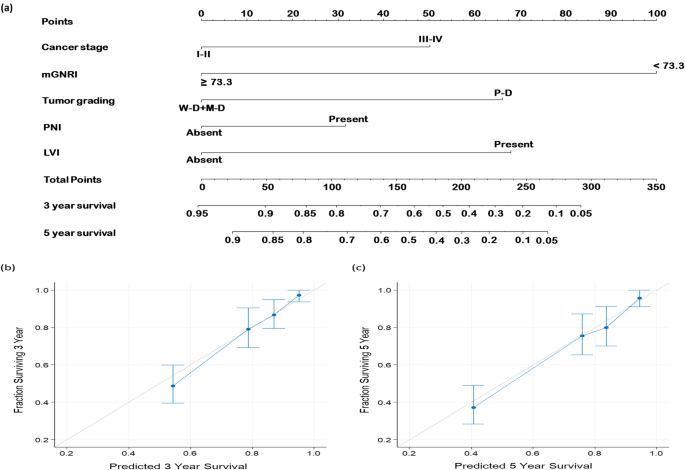
Predictive nomogram.One) Nomogram designed to predict OS based on mGNRI and independent prognostic factors identified by multivariate analysis. The contribution of risk level of each variable is shown by a line segment and its corresponding point. Total points were calculated by summing the points of each variable. Vertical lines were drawn from the calculated total points to determine the probability of 3- and 5-year OS. (b) 3 years and (c) 5-year OS is shown. The light grey line at a 45 degree angle represents perfect predictive accuracy, and the blue line represents the prediction results of the nomogram. The performance of the nomogram is shown as blue dots with bars, along with the 95% confidence interval for OS prediction. 56 yearsLymphatic vascular invasion, medical doctorModerate differentiation, GNRIModified Geriatric Nutritional Risk Index, PDInsufficient differentiation, IndividualPerineural invasion, WDIt is well differentiated.