Chance Dean was alive for just 25 days.
Yet his tragic story has reverberated in hospitals around the country, impacted the stock price of two multinational corporations, and ignited a high-stakes legal clash over a pernicious disease that kills hundreds of babies a year in the United States.
Born two months early and weighing less than four pounds, Chance spent all his days under close medical supervision in neonatal intensive care units (NICUs) near his family’s home in Southern Illinois.
His mother, Jasmine Watson, was unable to produce enough breast milk to fully nourish Chance and his fraternal twin brother, Chase. She initially opted to have her sons fed with a combination of her own milk and human breast milk from donor banks.
As Chance and his brother were being prepared for transfer to a hospital where donor milk was unavailable, doctors began transitioning them on Day 12 to a formula designed specifically for premature, low-birthweight infants, in addition to Watson’s breast milk, which was fortified to adequately support their nutrition.
On Day 22, Chance took a sudden turn for the worse.
“He just seemed like he just didn’t feel good,” Watson, 25, said in an interview. “It seemed like he was uncomfortable.”
Doctors diagnosed Chance with necrotizing enterocolitis (NEC, pronounced “neck”), a devastating illness of the intestines that primarily affects premature infants. The disease led to three urgent surgeries in an unsuccessful effort to save his life.
At 9:43 p.m. on March 28, 2020, Chance died in the arms of his mother.
“In that moment, I felt like the only thing that I could do for him was be there,” Watson said. “I held him the entire time until his heart stopped beating.”
Chance’s twin, who received the same formula at the same time, did not develop NEC.
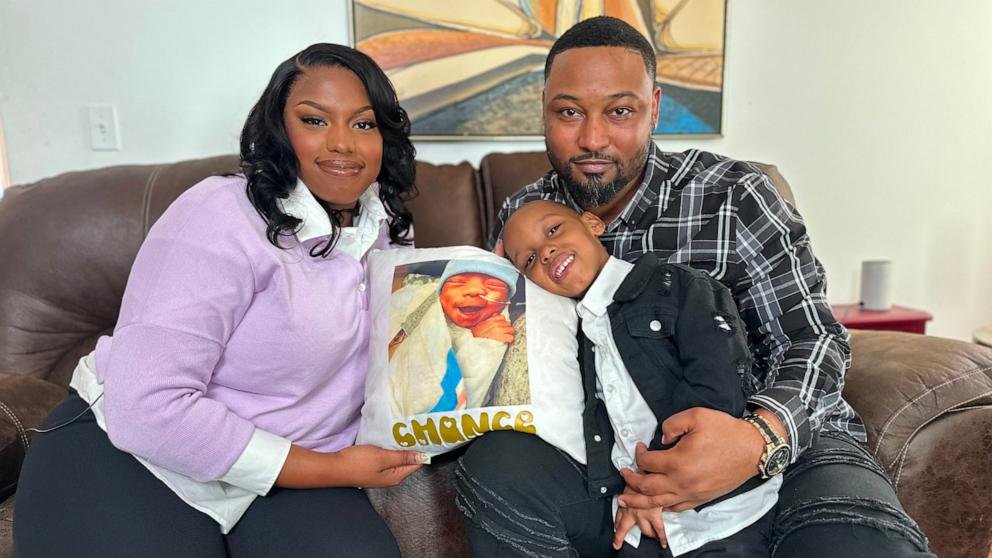
Four years later, a photograph of Chance — in a tiny blue knit cap — was displayed for jurors as “Plaintiff’s Exhibit 887” at the St. Clair County Courthouse in Belleville, Illinois. Watson alleged in a civil lawsuit that Chance’s NEC developed because of the switch from donor breast milk to a cow’s milk-based formula made by Mead Johnson, a global pediatric nutrition company.
“The reason we’re here in this courtroom is because Chance Dean never made it out of the hospital,” Watson’s lawyer Sean Grimsley said in his opening statement. “He died because he was given formula manufactured and sold by defendant Mead Johnson.”
Phyllis Jones, a defense attorney for Mead Johnson, stepped up to tell jurors that Watson’s lawyers were unjustifiably pinning the blame for Chance’s death on the formula. “It’s an easy answer, but it’s not the right answer.” Jones said. “It’s not the answer that the evidence will ultimately support in this case.”
“Four different neonatologists at two different hospitals made the decision that preterm infant formula … was the right option for Chance Dean to keep him growing, to keep him developing,” Jones said.
After a three-week trial, the jury decided that the company was negligent and had failed to adequately warn Watson that the incidence of NEC is higher in formula-fed premature babies. The jury awarded Watson $60 million to compensate for her loss and for the suffering Chance endured.
“For good reason, we believe this is the largest compensatory damages award ever in St. Clair County and stands as one of the most substantial in Illinois state history,” Watson’s lawyers wrote in a press release following the verdict.
Mead Johnson , in a statement from its UK-based parent company Reckitt Benckiser, said it was “surprised and deeply disappointed with the verdict” and vowed to “pursue all options” to have it overturned.
“It is important to note that this is a single verdict in a single case and should not be extrapolated,” the statement said. “We continue to believe that the allegations from the plaintiff’s lawyers in this case were not supported by the science or experts in the medical community.”
The company told ABC News that the verdict “sets a dangerous precedent that interferes with the practice of medicine and the patient-doctor relationship.”
‘Warning moms’
The Watson case, which concluded in March, was the first of its kind to go to trial. Interest in the proceedings was so expansive that an overflow courtroom was opened to accommodate all the lawyers from around the country who came to observe.
That’s because there are more than a thousand similar lawsuits in the U.S., involving over 7,000 families whose premature babies died or suffered serious injuries from NEC — with the first NEC case against formula-maker Abbott, Mead Johnson’s chief rival, scheduled to go to trial Monday in St. Louis.
The lawsuits allege the cow’s milk-based preterm infant formulas made by Mead Johnson and Abbott cause or substantially increase the risk of premature infants contracting NEC, when compared to babies who are fed a diet of their mother’s own milk or donated breast milk.
“Our allegation is that these formula manufacturers should be, at minimum, warning moms, doctors, dietitians, nurses, and hospitals of the risk of this horrendous disease that comes with switching preterm infants from a human milk to a cow’s milk-based formula,” said Ben Whiting, a partner at Keller Postman, a national law firm that represents Watson and hundreds of other plaintiffs suing the companies.
Over the past three years, claims against one or both formula-makers have been filed in state courts from Connecticut to California. Hundreds more are pending in federal court. Plaintiffs argue that the companies have long been aware of the risks but have failed to provide adequate warnings to parents and their medical providers.
“We were never given any information about additional risk with formula,” said Brent Rheinecker, whose premature baby daughter Willa died from NEC four years ago. Brent and his wife Elizabeth filed suit against the formula makers in Madison County, Illinois. Their case has not yet been set for trial.
“We never want another family to go through what we did. We never want another child to go through what our baby did. Her life was so short,” Elizabeth Rheinecker said.
In their legal complaints, lawyers for the families suing Mead Johnson and Abbott cite several scientific studies spanning three decades that have reported a higher occurrence of NEC in formula-fed preemies. The magnitude of the risk, however, varies widely in the scientific literature — from no significant difference to as much as three to ten times greater. Still, no study to date has shown that formula causes NEC.
Recent research, published in January in the Journal of the American Medical Association, followed 483 extremely preterm infants and found that babies in a preterm formula group gained weight more rapidly than those fed only with nutrient-fortified human donor milk — but that over twice as many formula-fed babies (9.0% compared to 4.2%) developed NEC compared to those fed only with donor milk. Health care providers say this is not enough to show a conclusive cause, but enough for scientists to continue to study the association. At the same time, some premature babies who were never given formula went on to develop NEC, suggesting that human milk is not completely protective.
“What we’re trying to do is to make sure that moms and doctors have the complete information that they need in order to make the best decision possible that they can for their preterm babies,” Whiting said. “The pain and suffering that these babies go through with this NEC is absolutely enormous. The way that it tears families apart — even if you’re a strong mom like Jasmine Watson — is significant.”
The lawsuits targeting the preterm formulas do not allege that the products are contaminated. The litigation is unrelated to Abbott’s baby formula recalls in 2022, which led to nationwide shortages.
‘An essential part of the medical toolkit’
Mead Johnson and Abbott, direct competitors in business, have been largely aligned in defending their respective preterm formulas, which they describe as “essential, safe, life-saving nutrition products” that have been successfully administered in NICUs for decades, according to court filings. The companies contend the mass litigation is itself “causing fear among parents” and “endangering the relationships” between parents and their physicians.
“No published study has ever concluded that defendants’ products cause NEC,” attorneys for the companies wrote in a joint filing in federal court. “Despite plaintiffs’ recent campaign against these products, NICU medical teams — including in the world’s best hospitals — continue to administer them as an essential part of the medical toolkit for treating these most fragile of patients.”
Amy Gates, a pediatric nutrition specialist who serves as Mead Johnson’s medical director, said in an interview after the Watson verdict that plaintiffs’ attorneys are “taking advantage” of the emotional impact that comes with the loss of a child.
“My fear is that we lose sight of the science and we allow emotion to win. And if that happens, there will be thousands of preemies who will be at risk,” Gates said. “Not every baby can sustain himself on just breast milk. And loss of access to these life-saving products would be a tragedy.”
The two companies have also argued that because their preterm formulas are used almost exclusively under medical supervision in hospital settings, they should therefore be considered by courts in the same manner as prescription medications and medical devices, where a legal principle known as the “learned intermediary doctrine” often applies. The logic of the doctrine is that medical professionals — the learned intermediaries — are best positioned to know the risks and benefits of a particular treatment and to communicate that to patients.
Three courts, however, have rejected that argument, declining to apply the doctrine to preterm infant formula, because – as one judge wrote – “it is not a recognized prescription medication or medical device.”
“At the end of the day, it’s the formula manufacturer — it’s their product. And so they are the ones that actually know the risks of using their own product,” Whiting said.
The presiding judge in the Watson case, in a pretrial ruling, rejected the learned intermediary defense and later instructed the jury — over Mead Johnson’s objections — that the company had a duty to warn “the consumer, like Jasmine Watson, about the dangers of its products,” according to court records.
Mead Johnson contends that jury instruction severely undercut their defense. The company argued at trial that it had no legal obligation to warn Watson or other patients, because the doctors who administer preterm formula already know about the risks of NEC.
“These patients are cared for by highly trained neonatologists and dietitians and clinical staff that know what they’re doing,” Gates said. “They fully understand the risks and benefits of everything they do for these patients.”
But Watson’s lawyers argued that testimony from doctors at trial indicated they did not fully appreciate the degree of risk allegedly associated with preterm formula.
“The doctors in this case talked about how there was a slight increased risk of NEC by switching to the formula, when in fact it’s a significant risk,” Whiting said. “And the doctors, they are not omnipotent. They don’t know everything there is to know about everything that’s out there. And that’s why at the end of the day, the legal duty on the manufacturers is to make sure to do everything that they can to make sure that the mom knows about the risk. And one of the ways they can do that is by giving a better warning to the doctors.”
‘A tragic disease’
NEC is a life-threatening intestinal disease predominantly impacting young neonates born prematurely, though it affects older and full-term babies in less common instances. Many infants recover, but the condition can lead to death or lifelong medical issues in the most severe cases.
“Babies who are born preterm, particularly those that are born with a birth weight less than three pounds, or who are very low birthweight, are at risk of a number of complications related to prematurity. That doesn’t just include NEC. It can also include their lungs and their brain,” said Dr. Ravi Patel, a neonatologist at Children’s Healthcare of Atlanta.
Patel, an assistant professor of pediatrics at Emory University, has been studying NEC for 14 years.
“It involves the sudden development of intestinal inflammation, and in severe cases, it can go on to where the tissue dies, and babies need surgery,” Patel said. “NEC is a tragic disease. But most people have never heard of NEC and don’t know what it is, even though it is a major contributor to neonatal mortality.”
The exact number of infants who have had NEC is unknown, but research shows the incidence of NEC has declined over the last 20 years. One recent study published in the Journal of Pediatric Surgery found that on average, there were about 3,000 cases a year from 2006 to 2017. Despite similar declines in mortality rates, data from the Centers for Disease Control and Prevention (CDC) shows that from 2017-2021, over 300 infants died from the disease each year, on average.
The cause of NEC is unknown, though it is believed to be a combination of multiple risk factors, the most important being premature birth and very low birthweight. Other possible factors include “the makeup of bacteria in the intestines, not enough blood flow or oxygen to the intestines, and an infant’s diet,” according to the American Academy of Pediatrics (AAP).
“NEC is a multifactorial disease. It’s not just any single factor we can pinpoint to why babies develop NEC,” Patel said. “We know that babies who only get breast milk are still at risk.”
Though a definitive cause of NEC has not been determined, it has been shown that the use of breast milk can be protective.
“One of the best ways to prevent necrotizing enterocolitis is by breastfeeding,” said Patel, who is not involved in any of the litigation related to NEC. “Our goal is to always provide mother’s own milk, but when that’s not possible, the feeding choices involve donor milk as an option. And donor milk has been shown, particularly in recent studies, to lower the risk of NEC.”
An AAP policy statement in 2012 noted that “feeding preterm infants human milk is associated with a significant reduction (58%) in the incidence of necrotizing enterocolitis” and recommended that “all preterm infants should receive human milk.” When mother’s own milk is unavailable “pasteurized donor milk, appropriately fortified, should be used,” the statement said.
Donor milk comes from mothers who have pumped more breast milk than they need. That milk is then collected and processed by networks of volunteers. Donor milk and maternal breast milk are typically fortified with extra calories and nutrients to meet the unique needs of premature infants in NICUs. Studies have also indicated that the pasteurization process — which kills bacteria and viruses that might be in the donor milk — may reduce many of the protective components of human milk.
“Overall, pasteurized donor milk is nutritionally suboptimal to a mother’s own milk,” according to an AAP clinical report published in 2021.
The Human Milk Banking Association of North America and its 33 milk banks dispensed nearly 10 million ounces of donor milk to 1,500 hospitals in 2023, the organization announced in February, but added that “the need for donor human milk continues to grow.”
An analysis by the CDC found that donor milk was unavailable for very-low-birthweight infants at 13% of advanced care NICUs, based on data from 2020. “Availability of donor milk at hospitals might be affected by supply from milk banks, cost, and reimbursement, which can vary by state and payment source,” the report said.
“Because donors’ milk is a limited resource, some babies do need formula to provide adequate nutrition,” Patel said. “We want to provide nourishment to babies, to make sure that they grow, that they get bigger, and ideally, that they can go home with their families.
“And those nutrition decisions are made at the bedside between clinicians and families, taking in the context of the unique circumstances of each baby,” he added.
‘Can’t be replicated’
Attorneys for Mead Johnson argued during Watson’s trial that the reason for differences in NEC rates is “not because formula is harmful. It’s because formula doesn’t protect in the same way that breast milk does. It doesn’t include the same protective factors.”
“We at Mead Johnson acknowledge that mother’s breast milk, in particular, is unique in its biologic protections that can’t be replicated,” Gates said. “Not every baby has access to breast milk. And there are many reasons why babies need alternatives and supplements. And we believe that access to safe and nutritious formula is extremely important. And loss of that access could put thousands of preemies at risk.”
The verdict in Watson’s lawsuit propelled the burgeoning legal dispute into international headlines and jolted the companies’ stock prices. Reckitt lost billions in market value following the jury’s decision in March, while Abbott shares dipped about 4% over two days.
Reckitt’s CEO, Kris Licht, told analysts during an earnings call in April that the company had “no plans to stop providing the product, as that would be detrimental to the care of preterm babies and their families.”
“I can tell you that we are spending a lot of time thinking about how to best navigate the litigation; how to prevail in the litigation,” Licht said.
The trial’s outcome also prompted a cautionary public statement from the NEC Society, a nonprofit patient-led advocacy group, urging against abrupt changes to neonatal care based on a single jury’s findings.
“Neonatal feeding decisions should be made at patients’ bedsides, not in courtrooms,” the organization said. “Verdicts like the Watson case may prompt ICUs to reconsider their approaches to feeding neonatal patients, but not necessarily in a way that better protects infants from NEC.”
Peter Pitts, a former U.S. Food and Drug Administration official, in an opinion article published in the Washington Times, argued that the litigation presents “a direct threat to the lives of America’s preterm infants.”
“Once again, tort lawyers, sensing a big payday, have put greed before civic duty by putting at risk one of our most at-risk populations – premature infants,” wrote Pitts, the founder of the nonprofit Center for Medicine in the Public Interest.
‘I would have made a different decision’
Watson said that she could not recall anyone talking to her about an elevated risk of NEC before her two sons were transitioned to formula and transferred to the hospital that did not use any donor breast milk.
“If I had known the risk of giving my children this formula, absolutely, I would have made a different decision,” she said. “I don’t want any other parents to ever have to go through that. I want them to know that you can ask questions. Make sure you understand.”
Two months after the conclusion of Watson’s case, Mead Johnson filed a motion for a new trial, arguing that the judge erred by precluding the company from presenting evidence of potential contributing causes of Chance Dean’s death, including an alleged accidental laceration or abrasion of his liver during the second of his three surgeries. The company also contends the jury instructions “erased the important role of physicians in making decisions for premature infants in the neonatal intensive care unit.”
Watson’s attorneys argue in response that the company’s motion is “unfounded, and should be quickly denied so Mead Johnson can be finally held accountable for its actions, and so Chance Dean’s family can finally get the justice and closure they deserve,” according to court records.
“Despite the lengthy adversarial process and the resulting lawful jury instructions, Mead Johnson wants to lay blame for the jury’s verdict at the feet of this Court and not its own negligence or its own failure to warn,” Watson’s lawyers wrote.
The court has set a hearing on Mead Johnson’s post-trial motion for later this month.
Meanwhile, the first NEC case against Abbott is scheduled to go to trial on Monday, with the plaintiff, Margo Gill, alleging that her daughter suffered long-term health consequences from NEC, which she blames on the company’s preterm infant formula. Abbott has denied the allegations.
“These cases seek to advance a theory promoted by plaintiffs’ lawyers that has no basis in science and is not supported by the medical community. The allegations are without merit,” said Scott Stoffel, a vice president of public affairs for the company.