A single-center randomized trial showed that acupuncture improved sleep quality in people with Parkinson’s disease.
After 4 weeks of treatment, patients who received real acupuncture and those who received sham acupuncture had significant increases in the Parkinson’s Disease Sleep Scale (PDSS), increasing by 29.65 and 10.47 points from baseline, respectively (PBoth were less than 0.001, but only the acupuncture treatment group showed an increase of 25.35 points over the 8-week period, and the effect was sustained (P<0.001), compared with 5.68 points in the placebo group (P= 0.03), reported Lixing Zhuang, PhD, of the First Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine in China, and his co-authors.
“We tentatively conclude that although sham acupuncture may induce a short-term placebo effect, acupuncture provides lasting clinical benefit in improving subjective sleep quality in patients with Parkinson’s disease,” they wrote. JAMA Network Open“In this study, the placebo effect of acupuncture diminished over time, but the therapeutic effects persisted over the long term.”
Sleep disorders are common in Parkinson’s disease patients, occurring as a side effect of the disease progression or treatment, and previous studies have shown that lack of sleep can accelerate the deterioration of gait and dyskinesias, as well as the progression of mood and cognitive symptoms.
According to Juan and team, there are no other large randomized clinical trials focusing on acupuncture for Parkinson’s-related sleep disorders, but an open-label pilot study established safety and tolerability and improved sleep in 20 Parkinson’s patients. A randomized clinical trial of 30 patients showed that electroacupuncture improved PDSS and Nonmotor Symptom Scale (NMSS) scores.
“The study used a single validated questionnaire to arrive at its primary outcomes, so we’re not seeing a clear path to success,” said Shirin Shafazand, M.D., of the University of Miami, who was not involved in the research. Medpage Today “The study was not designed to evaluate the impact of acupuncture as an add-on therapy on different aspects of sleep quality, such as whether acupuncture improves insomnia symptoms or overall impression of sleep refreshment or pain or stiffness.”
Although the differences in sleep quality were statistically significant, “it is also unclear whether the reported differences in sleep quality are clinically meaningful,” she added. She recommended replicating similar studies elsewhere, with larger numbers of people and more sleep parameters.
For this study, participants were recruited from the Parkinson’s Disease Clinic of the First Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine between February 2022 and February 2023. Participants were required to be aged between 20 and 80 years, diagnosed with idiopathic Parkinson’s disease, complaining of moderate or severe sleep disturbance or a PDSS score below 110 (score ranges from 0 to 150, increasing as sleep quality improves), Hoehn and Yahr Scale stages 1 to 3, and taking Parkinson’s disease medication continuously for 30 days.
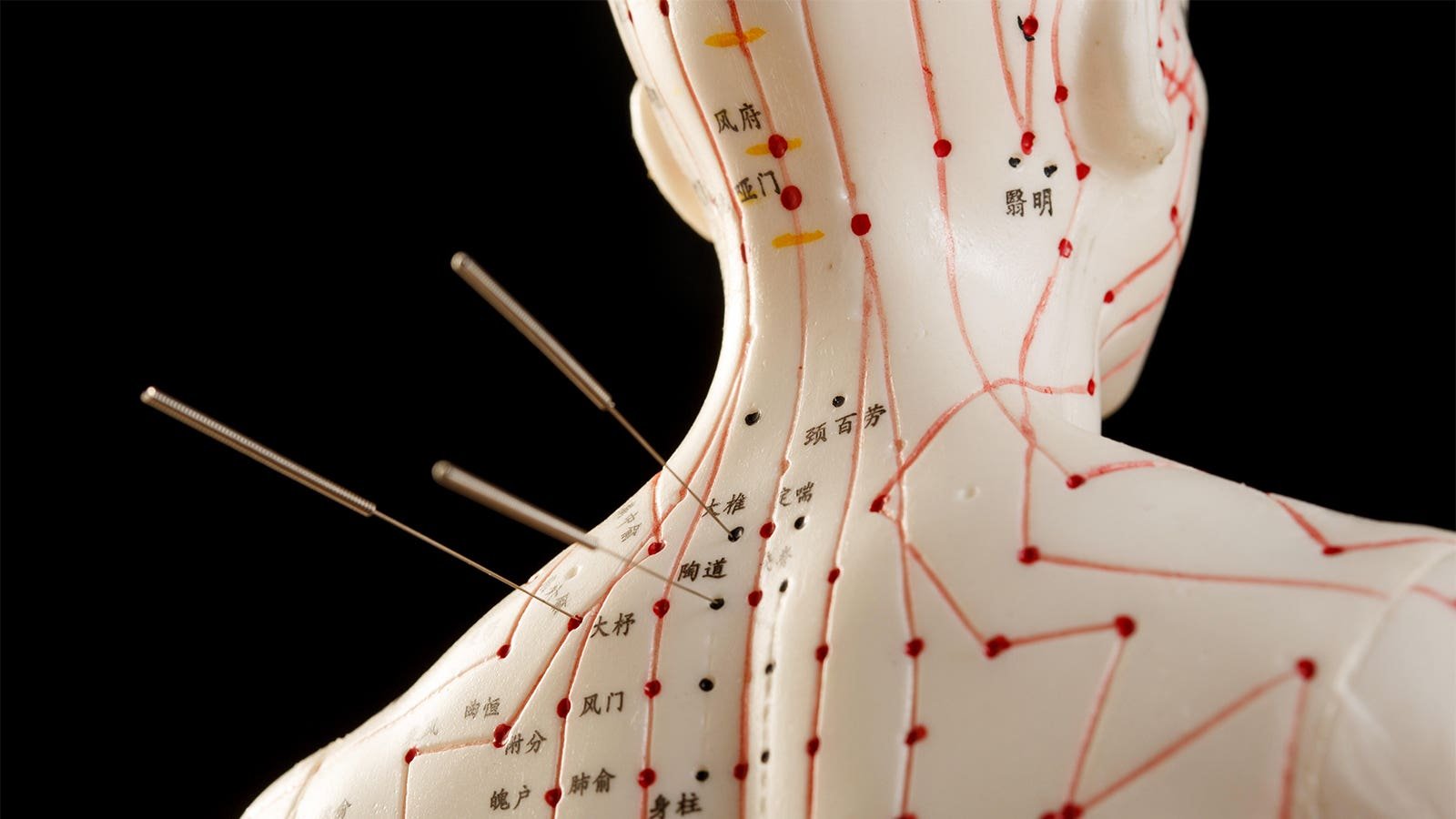
All patients were given sleep hygiene instructions. The acupuncture group received real acupuncture, and the sham acupuncture group received stainless steel needles that did not penetrate the subcutaneous tissue for 30 minutes, three times a week for four weeks. Both groups used the same 10 acupressure points on the head, hands, feet, and legs.
Of 83 participants enrolled, 78 completed the intervention and 4-week follow-up. Mean age was 64 years and 52.6% were male. Most participants had a Hoehn and Yahr stage < 2.5 and the mean baseline PDSS score was 85.3.
Secondary outcomes included excessive daytime sleepiness, anxiety, severity of non-motor symptoms, severity of motor symptoms, and quality of life. The group that received actual acupuncture showed significant improvements in motor and non-motor symptoms, sleepiness, anxiety, and health-related quality of life scores after the intervention.
No serious adverse events were recorded in either group. The most common adverse events associated with acupuncture were self-reported severe tremors, bleeding, numbness, infection, or sharp pain during treatment.
Zhuang and colleagues acknowledged that their study had several limitations. Due to the nature of acupuncture, acupuncturists were not blinded, and follow-up was only four weeks, which may have limited assessment of the long-term effects and durability of treatment. Participants were recruited from specialized Parkinson’s disease clinics in China, which likely limits the generalizability of the study findings.
Disclosures
This research was funded by the National Natural Science Foundation of China, the Guangdong Provincial College and University Innovative Research Team Project, and the First Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine.
Zhuang said he had no conflicts of interest. His co-authors hold a patent on the dummy needles used in the study.
Shafazand had nothing to disclose.
Primary information
JAMA Network Open
Citation reference: Yan M, et al. “Acupuncture and Sleep Quality in Patients with Parkinson’s Disease: A Randomized Clinical Trial.” JAMA Netw Open 2024; DOI: 10.1001/jamanetworkopen.2024.17862.

![author['full_name']](https://clf1.medpagetoday.com/media/images/author/Putka_Resize_96.jpg)