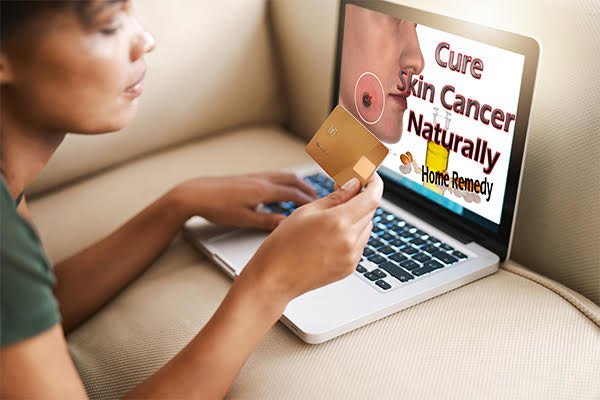
According to previous estimates, approximately 85% of skin disease patients in the United States use alternative treatments such as herbal, vitamin, and mineral supplements. Although the majority of skin cancer patients receive conventional treatment under the direction of a dermatologist, some patients use only alternative herbal remedies instead.1
Unfortunately, there is little reproducible evidence to support the effectiveness of these plants against skin cancer, and patients who choose unproven alternative treatments are often discouraged from starting conventional treatments with proven efficacy. Often delayed.1 The U.S. Food and Drug Administration (FDA) does not regulate herbal supplements, but it does address the issue of deceptive cancer treatments on its website.2

Janet Y. Lee, MD, and Jeremy T. Kump, MD, of the Department of Dermatology at the University of Washington School of Medicine in Seattle, recently published the results of a literature review of common topical herbal treatments touted as treatments for skin cancer. We started by searching for the following terms: “non-melanoma skin cancer,” “basal cell carcinoma,” “squamous cell carcinoma,” and “melanoma.”1 The authors then applied the level of evidence and grade of recommendation determined by the Oxford Center for Evidence-Based Medicine.
Do these herbal supplements really work?
Doctors. Lee and Kamp reviewed several herbal supplements for skin cancer and provided background information on each. Here’s what they reported on eight popular supplements: (Unfortunately, for those who believe in these products, the author’s findings can only be described as sobering.)
black ointment
The main ingredients of black ointment, Rhizoma and zinc chloride, cause local tissue necrosis. Black ointment is currently being marketed by companies based outside the United States as a treatment for melanoma and non-melanoma skin cancer, despite FDA warnings to discontinue it. Sanguinarine, an active ingredient in red root herb, has been shown to induce apoptosis and cytotoxicity in melanoma cells in mouse models, but no clinical trials have investigated its efficacy and safety. However, there have been numerous case reports of serious side effects from treating skin cancer with black ointment.
Of published case reports on black ointment treatment of basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma lesions in 13 patients, 8 BCC lesions and 1 SCC lesion showed complete response (6 had biopsy-proven results). Metastases were seen in 2 cases each of residual and advanced BCC, 2 cases of melanoma, 1 case of SCC, and 1 case of BCC. Almost all patients experienced serious side effects, including pain, ulceration, and scarring.
evaluation: Given the inconsistent evidence and severity of side effects, the black ointment scores D recommendation.
Sorasodine rhamnosyl glycoside
These glycosides come from the Solanaceae family, including tomatoes, potatoes, peppers, and eggplants. They attach to the surface of cancer cells but not to normal tissue and initiate apoptosis. Creams containing solasodine rhamnosyl glycosides are approved for use in Australia and the United Kingdom, but not in the United States.
A case series (total of 86 patients) and one randomized controlled trial (RCT) (N=94) were found in the literature. In a case series of 86 patients followed for 3 months, complete regression was seen in 100% of BCC, SCC, and actinic keratosis cases after approximately 5 weeks of treatment. In an 8-week RCT of 94 BCC patients, 66% of patients who used a cream containing solasodine glycosides showed histologically confirmed BCC clearance. However, 22% of these patients had BCC recurrence during the study’s 1-year follow-up. No serious side effects have been reported.
evaluation: Solasodine glycosides have inconsistent results; D recommendation.
frankincense
Frankincense, derived from the Boswellia tree, contains boswellic acid, which induces apoptosis as shown in animal studies. In humans, only one case study of a middle-aged man with two BCC lesions has been reported in the current literature review. After his 4 months of treatment with frankincense oil, his one lesion on the patient’s arm completely resolved and one on his chest showed localized residual BCC. Treatment-related allergic contact dermatitis has been reported.
evaluation: Since only one case study was found, frankincense D recommendation.
cannabis
Cannabinoids have shown melanoma and non-melanoma antitumor effects in preclinical studies in mouse and human melanoma cell lines. Among the results are that synthetic cannabinoids cause apoptosis, impaired angiogenesis, and inhibition of epidermal growth factor receptors, as well as reduced adhesion of melanoma cells to brain endothelial cells and transendothelial migration of melanoma cells. It also includes the possibility of failure. Tetrahydrocannabinol (THC) was shown to induce apoptosis and reduce cell viability in melanoma cells, and also demonstrated reductions in melanoma cell proliferation, angiogenesis, and metastasis.
evaluation: Different brands of cannabis oil are touted for treating a wide range of medical conditions, from multiple sclerosis to depression, but there are no clinical trials to back up the claims. Therefore, this lack of clinical evidence has led to the topical use of cannabinoids. D recommendation.
black raspberry
In the only skin cancer study to date, the use of black raspberry extract after UVB exposure reduced the number and size of skin cancer tumors in mice. However, no clinical trials have been conducted on humans, and no side effects associated with black raspberries have been reported.
evaluation: Due to the lack of clinical evidence, the use of black raspberry extract is (you guessed it) D recommendation.
milk thistle
Silibinin, a flavonoid isolated from milk thistle seeds, induces apoptosis in mouse BCC cell lines and inhibits the growth of mouse BCC tumors. Although milk thistle or its active compounds have been reported as a treatment for skin cancer, no human clinical trials have been conducted. No adverse effects have been reported with topical milk thistle.
evaluation: As with several other skin cancer herbs evaluated, Dr. Lee and Kampf found no clinical evidence of the effectiveness of milk thistle or its active compounds. that too, D recommendation.
st john’s wort
Hypericin is an active ingredient in St. John’s wort that induces apoptosis in human melanoma cell lines and SCC cells when administered before photodynamic therapy. A pilot study conducted on 34 patients showed that after weekly treatment with St. John’s wort extract and 6 weeks of photodynamic therapy, 50% of 8 patients with actinic keratosis and 28 of 21 patients with BCC %, it was shown that 40% of BCC patients had a complete clinical response. Five patients with non-invasive SCC. However, no RCTs have investigated the efficacy or safety of St. John’s wort in treating skin cancer.
evaluation: The jury is still out as there is no conclusive evidence of effectiveness. Therefore, the topical use of St. John’s wort for skin cancer received yet another score. D.
Turmeric
Curcumin, a derivative of turmeric, induces apoptosis in preclinical studies and inhibits melanoma cell migration and invasion in vitro. However, there are no clinical studies showing that curcumin is effective in treating non-melanoma skin cancer. Allergic contact dermatitis, contact urticaria, and pruritus have been reported with topical use of turmeric.
evaluation: another D This is also due to a lack of clinical evidence.
fake, fake, fake
Despite some support from preclinical data, there is little clinical evidence to support the use of these plants for skin cancer treatment. So why do patients keep buying them? The authors state: “Many websites and patient testimonials cite distrust of doctors as a reason for turning to alternative treatments, often ignoring the potentially devastating consequences. It is important to be aware of alternative treatments and maintain an open dialogue with patients.”
They note that while doctors and other medical professionals have reported “some encouraging results with herbal preparations, the positive results are not reproducible and are not strong enough to replace current standard treatments.” “Patients should be warned that this is the case.” . . These plants can cause indiscriminate local tissue destruction. . . It can result in incomplete healing and delayed diagnosis, leading to further disease progression locally at best and metastasis at worst. ”
release date: