1 Introduction
Postpartum Stress Urinary Incontinence (PSUI) refers to the occurrence of urinary incontinence after pregnancy or childbirth. The main symptoms are urine leakage from the urethra when the maternal abdominal pressure increases, such as coughing, sneezing, laughing, walking or running. Symptoms stopped immediately after stopping these actions (1). The causes of PSUI are mainly related to the hyperextension or injury of pelvic floor muscles, surrounding connective tissues and pelvic floor nerves during vaginal delivery. Risk factors associated with PSUI included higher maternal body mass index (BMI), age, delivery time, vaginal delivery, surgical vaginal delivery, perineal or anal sphincter trauma, and higher birth weight (2–6). According to relevant studies, the incidence of stress urinary incontinence is about 19% after 6 weeks (7). In a systematic review of population-based studies, 33% of women experienced urinary incontinence within the first 3 months after giving birth (8). A longitudinal cohort study showed that the prevalence of stress incontinence reached 42% in 241 women 12 years after their first birth. The prevalence of stress incontinence during the first pregnancy and 12 years after delivery was significantly higher in women who developed it during the first pregnancy (56%) and shortly after delivery (78%) than in women without initial symptoms (30%), indicating an increased risk of long-term symptoms of stress incontinence occurring during the first pregnancy or puerperal period (9). This disease not only seriously affects the quality of life of patients, but also increases the psychological burden and economic burden of patients (10, 11). In order to allow the body to recover from pregnancy and childbirth, surgical treatment is usually delayed after delivery. Medication may not be appropriate for breastfeeding women (12). Stem cell research, which has risen to the forefront of regenerative medicine, has the potential to cure stress urinary incontinence but has not yet been approved for routine clinical usage (13).
Pelvic floor muscle-related symptoms may coexist with symptoms of pelvic floor disorders such as urinary incontinence, voiding dysfunction, fecal incontinence, defecatory dysfunction, sexual dysfunction, or pelvic organ prolapse, as well as coexist with other disorders of neuro-musculo-skeletal structures in the pelvis or spine (14). Studies recommend pelvic floor rehabilitation training as the first choice for conservative treatment of stress incontinence (15). The Chinese Guidelines for the Diagnosis and Treatment of female stress Urinary Incontinence (2017) recommend pelvic floor muscle training as a first-line non-surgical treatment, with efficacy somewhat similar to surgery and without any risk (1). Pelvic floor rehabilitation training can effectively alleviate postpartum pelvic floor dysfunction and reduce symptoms of urinary incontinence. New study found that pelvic floor rehabilitation training protocol reduced urinary incontinence in pregnant women. The program allowed significant improvement in the quantity of urinary leakage and an increase in the strength of the pelvic floor muscle (16). Conventional pelvic floor rehabilitation methods mainly include Kegel pelvic floor muscle training, Biofeedback training, low-frequency bioelectrical stimulation, and the use of vaginal dumbbell (17). However, the poor compliance of patient’s leads to poor recovery effect is a common phenomenon in society. It is often due to factors such as inability to adhere to a family exercise plan, inconvenience in daily activities, worry about children, uncertainty about efficacy, and financial burden (18). Therefore, the effect of single treatment is limited (19).
Acupuncture, as an important traditional Chinese medicine treatment, has been included in the Representative List of the Intangible Cultural Heritage of Humanity by the United Nations Educational, Scientific and Cultural Organization (UNESCO) and is considered safe and effective (20–22). Acupuncture is applicable to a wide range of diseases. In a systematic study that identified 133 acupuncture-related clinical practice guidelines and 433 acupuncture interventions published between 2010 and 2019, 380 recommended the use of acupuncture, and 43.2% of the 303 recommendations that used GRADE to determine the strength of recommendations were strong. Acupuncture is recommended in 87.8% of obstetrics, gynecology and women’s guidelines (23). Acupuncture has certain advantages in the treatment of PSUI, which can regulate the pelvic floor muscle through the stimulation of relevant acupuncture points, thus promoting the recovery of bladder function (24). In recent years, the integration of Chinese and Western medicine in treating various diseases has gained significant attention in research. Acupuncture combined with pelvic floor rehabilitation training has made certain progress in improving the clinical symptoms of PSUI patients (25–28), but there is still a lack of high-quality systematic reviews at home and abroad. Only one systematic review evaluated the effectiveness of acupuncture combined with pelvic floor muscle training for PSUI (29). The review has obvious flaws that threaten the veracity of their findings. Firstly, this study was not registered in the International Prospective Register of Systematic Reviews (PROSPERO). Secondly, it is found that the search scope was small, only 6 databases were searched. Thirdly, the methodological quality of the 12 included papers was very poor. Finally, acupuncture is treated as a whole, and the efficacy of acupuncture alone has not been systematically studied. From what we know, several new RCTs have been published since the meta-analysis was published.
In conclusion, there is no supporting evidence for acupuncture combined with pelvic floor rehabilitation training to improve the efficacy and safety of PSUI. This study collected domestic and foreign relevant clinical research literature for quality evaluation and meta-analysis, in order to provide scientific evidence for acupuncture combined with pelvic floor rehabilitation training to improve PSUI in clinical practice.
2 Methods and analysis
We constructed this protocol report and implementation review according to the guidelines for the Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P) 2015 (30).
2.1 Study registration
In accordance with the guidelines, our systematic review protocol was registered with PROSPERO on August 30, 2023 (registration number CRD42023455801).
2.2 Eligibility criteria
2.2.1 Study designs
We will only include randomized controlled trials (RCTs), excluding cross-sectional studies, reviews, case reports and systematic reviews.
2.2.2 Participants
We will include women who meet any of the diagnostic criteria or guidelines for postpartum stress incontinence and exclude patients with serious other psychiatric disorders. There will be no restrictions on the age, race, education level, course of disease, etc.
2.2.3 Interventions
The experimental group will include any kind of acupuncture therapy combined with pelvic floor rehabilitation training, including acupuncture, moxibustion, electroacupuncture, warm acupuncture, etc. Non-acupuncture combined with pelvic floor rehabilitation training intervention, such as acupuncture combined with pelvic floor rehabilitation training combined with massage, Chinese medicine, nursing and other confounding factors will be excluded.
2.2.4 Comparators
The control group will only be included in the simple pelvic floor rehabilitation training, including Kegel pelvic floor muscle training, Biofeedback training, low-frequency bioelectrical stimulation, vaginal dumbbell (17, 31).
2.2.5 Outcomes
Primary outcome: The primary outcome of this systematic review will be clinical effective rate.
Secondary outcomes: International Consultation on Incontinence Questionnaire-Short Form (ICI-Q-SF) (32), 1-h pad test, pelvic floor muscle potential value, incidence of adverse events will be included as secondary outcomes.
2.2.6 Language
We will only include articles reported in Chinese and English.
2.3 Search strategy
Randomized controlled trials (RCTs) of acupuncture combined with pelvic floor rehabilitation in the treatment of postpartum stress urinary incontinence will be searched in PubMed, Web of Science (WOS), Cochrane Library, EMBASE, China National Knowledge Infrastructure (CNKI), Chinese Biomedical Literature Database (CBM), Wanfang (WF), and VIP databases. The clinical trial Registry (ClinicalTrials.gov and Chinese clinical trial Registry) will also be searched. The search period will be limited to July 1, 2023, and the language limit of this systematic review will be Chinese and English. Subject words combined with free words will be used in the search. The search strategy for PubMed is shown in Table 1.
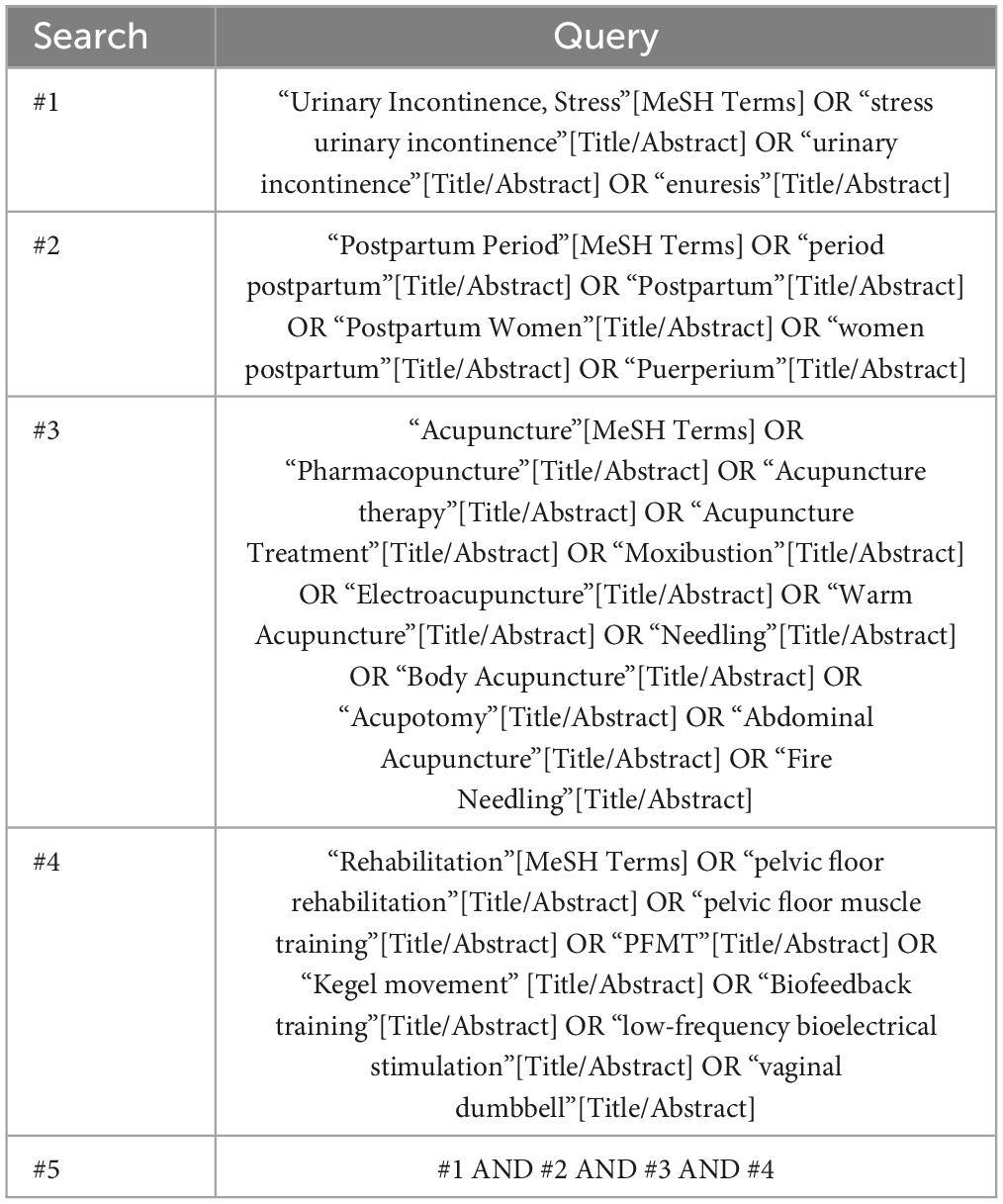
Table 1. Search strategy for PubMed.
2.4 Selection of studies
Two reviewers (WC and XD) will work independently on literature screening using Endnote software (V.X9.0). After reading the title and abstract of the literature, studies that do not meet the inclusion criteria will be removed. For studies that may meet the inclusion criteria, further review the full text to decide whether to include. In case of disagreement, a third reviewer (XG) will read and discuss it before making a decision. The process of study selection will be shown in a PRISMA diagram (Figure 1).
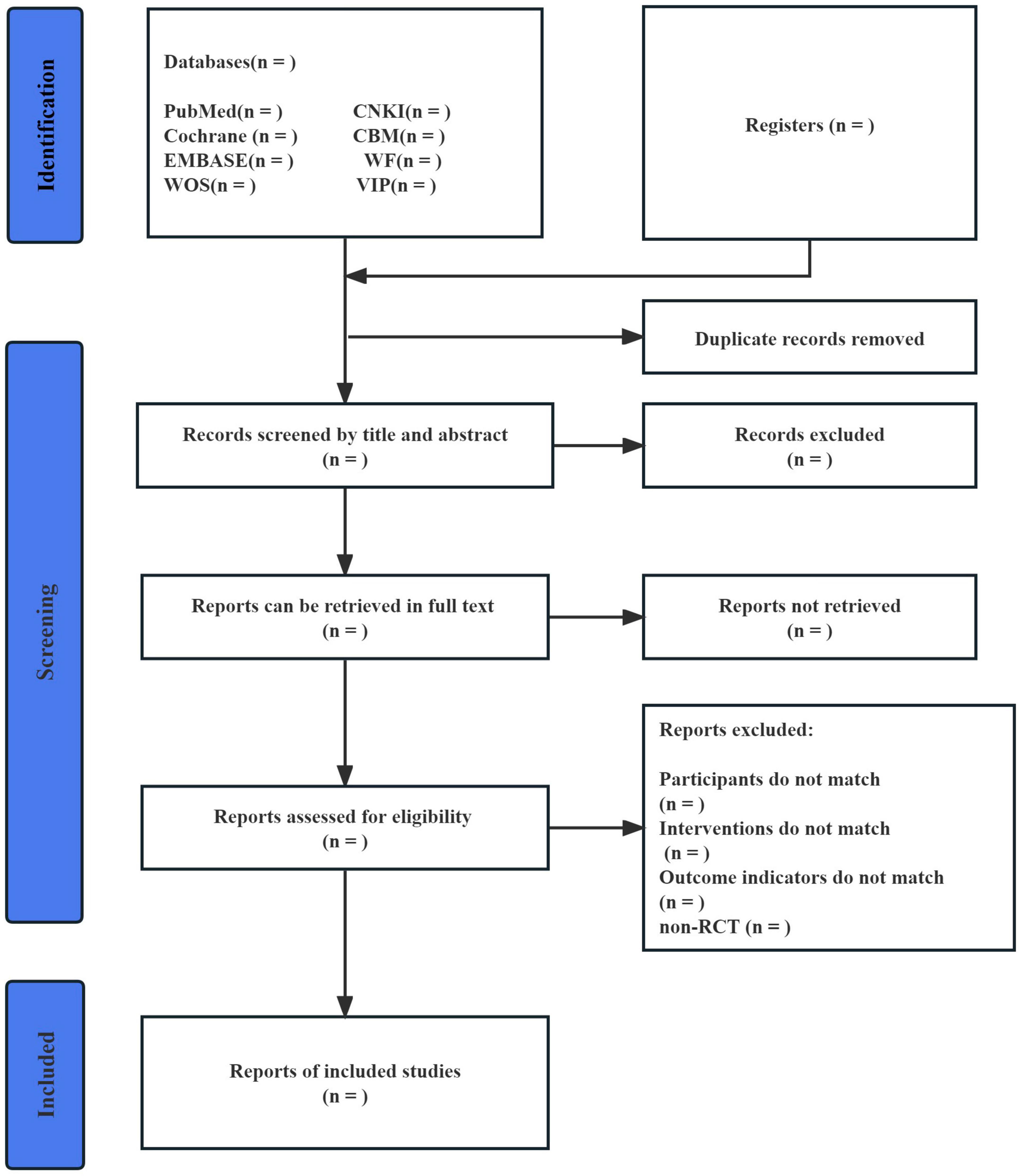
Figure 1. Flow diagram of study selection.
2.5 Data extraction and management
Data extraction and management will be completed by two reviewers (WC and XD) independently. If there is any inconsistency, two reviewers will check the original text at the same time and ask a third party arbitrator (XG) to discuss and solve it. Data will be extracted in a special data extraction table, including author name, year of publication, randomized method, diagnostic criteria, sample size, age of subjects, intervention measures, duration of treatment, and outcome indicators.
2.6 Quality assessment
The risk of bias will be assessed using the approach recommended by Cochrane Handbook for Systematic Reviews of Interventions (33). It will mainly include seven items: random sequence generation (selectivity bias), allocation concealment (selectivity bias), blinding of participants, carers or people delivering the interventions (implementation bias), blinding of outcome assessors (measurement bias), missing outcome data (attrition bias), selection of the reported result (reporting bias), and other sources of bias (other bias). Evaluate each case as “low risk,” “unclear risk,” or “high risk.” In the event of disagreement, the third reviewer will review and discuss it before reaching a decision.
2.7 Dealing with missing data
When missing data is available, we will make an effort to contact the original author of the study via email to obtain the necessary information. If not available, we will use sensitivity analysis to assess the impact on overall treatment efficacy of including trials with unreported intent to analyze treatment, high participant turnover, or other missing data.
2.8 Assessment of heterogeneity
We will assess the heterogeneity among the included studies. If P > 0.1 and I2 ≤ 50%, we will employ a fixed-effect model. If P ≤ 0.1 and I2 > 50%, indicating substantial heterogeneity among all groups, we will conduct subgroup analysis or sensitivity analysis to identify the source of heterogeneity. If heterogeneity is still high, a random-effect model will be chosen.
2.9 Data synthesis
For statistical analysis of each outcome, we will utilize RevMan 5.4, a statistical software provided by the Cochrane Collaboration. Continuous variables will be expressed as mean difference (MD), dichotomous variables as relative risk (RR), and 95% confidence interval (CI) will be used for each effect size. Statistical significance will be considered at P < 0.05.
2.10 Subgroup analysis and sensitivity analysis
We will use subgroup analysis to explore possible sources of heterogeneity, based on the following. (1) Patient characteristic (age, education level, severity of incontinence). (2) Types of acupuncture (Acupuncture, Electroacupuncture, Moxibustion, Body Acupuncture, Abdominal Acupuncture, Warm Acupuncture, Fire Needling, etc.). (3) Types of control group (Kegel pelvic floor muscle training, biofeedback training, low-frequency bioelectrical stimulation, vaginal dumbbells). (4) Duration (30 days vs. < 30 days).
If substantial heterogeneity persists following subgroup analysis, we will conduct a sensitivity analysis to evaluate the robustness of the pooled results. Studies deemed to have a high risk of bias, as well as studies with missing data, will be systematically excluded.
2.11 Assessment of publication bias
If the results of the meta-analysis include more than 10 studies, publication bias analysis will be performed using the funnel plot. P < 0.05 will be considered statistically significant.
2.12 Grading the quality of evidence
We will assess the quality of evidence using the Grading of Recommendations Assessment, Development, and Evaluation methodology (GRADE). All results will be divided into four levels: high, moderate, low and very low.
3 Discussion
With the implementation of China’s three-child policy in 2021, experts predict there may be a brief spike in the number of births. This may put some pressure on OB/GYNs in China (34). Therefore, the occurrence of PSUI has attracted much attention. Although PSUI is not life-threatening, it can seriously affect patients’ physical and mental health and quality of life (35). Traditional Chinese medicine believes that the occurrence of this disease is mainly caused by postpartum Qi and blood deficiency, kidney injury over time and damage bladder; gasification function. “Zhu Bing Yuan Hou Lun” said, “Because giving birth used a lot of Qi (energy), that may hurt the bladder function, and may lead cold air into the uterus system caused the vesical sac and bladder loses function, so enuresis And or manty are caused by difficulties in childbirth.” This disease should be treated with tonifying qi and tonifying kidney, receiving astringent and tonifying spleen and stomach. Acupuncture treatment of PSUI has the effects of tonifying deficiency and draining excess, regulating qi and blood, and balancing Zang-Fu Yin and Yang. New studies believes that acupuncture may promote the repair of pelvic tissue and bladder function by reducing serum relaxant and pelvic tissue transforming growth factor (TGF-β1) levels (36). Electroacupuncture stimulation can alleviate the signs of SUI, and its mechanism is related to the degradation of collagen in the anterior vaginal wall (37). Another study found that EA treatment changed the species composition of the intestinal flora in rats with SUI. Whether there is a link between the influence of EA on intestinal flora and the regulation of collagen metabolism is still unknown (38). The pelvic floor rehabilitation training can improve the pelvic floor blood circulation and muscle excitability by increasing the tension and contractility of the pelvic floor muscles, so as to relieve the symptoms of urinary incontinence. There was a study revealed that tremendous potential for the improvement of PFME education and targeting at-risk women in the peripartum period (39). Studies have shown that the combined treatment of PSUI can achieve mutual consolidation and prolong the curative effect. The significance of this systematic review is to provide evidence for clinicians to choose acupuncture combined with pelvic floor rehabilitation training to improve post-partum stress urinary incontinence.
Advantages of this study include: (1) This review will provide a comprehensive assessment of the efficacy and safety of acupuncture combined with pelvic floor rehabilitation training in the treatment of PSUI. (2) The search strategy of this review is comprehensive, and 8 databases and clinical trial registration platforms will be searched. (3) Outcome indicators consistent with clinical practice will be used in this study, including ICI Q-SF, 1-h urine pad test and pelvic floor muscle potential value.
There are still limitations to this study. (1) We will only search the Chinese and English databases, which may result in language sampling bias. (2) Due to the particularity of acupuncture operation, this review mainly considers the types of acupuncture, the experience and skills of acupuncture operators, and the specific acupuncture points are not limited. (3) Due to the limited literature available, the mechanism of PSUI cannot be discussed in depth in this review.
In future studies, the database of other languages should be increased to reduce language sampling bias. With the continuous research on PSUI, we should further explore the mechanism of its occurrence and the mechanism of acupuncture combined with pelvic floor rehabilitation training in the treatment of PSUI.
Ethics statement
Since we do not collect primary data for this systematic review, ethical approval is not required. The results of this protocol will be published in a peer-reviewed journal in accordance with PRISMA guidelines.
Author contributions
CW: Writing−original draft. DX: Writing−original draft. GL: Methodology, Writing−review and editing. LY: Formal analysis, Writing−review and editing. GX: Supervision, Writing−review and editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of the article. This systematic review is funded by the HSRP-DFCTCM-2023-3-14 and Special Project for Scientific Research on Traditional Chinese Medicine in Henan Province (NO.2022ZY1097).
Acknowledgments
We would like to thank all participants in this study for their contributions to this study. In addition, we would like to thank Dr. SETO PUI for revising the language section of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Urogynocology Subgroup, Chinese Society of Obstetrics and Gynocology, Chinese Medical Association. [Update of guideline on the diagnosis and treatment of female stress urinary incontinence (2017)]. Zhonghua Fu Chan Ke Za Zhi. (2017) 52:289–93. doi: 10.3760/cma.j.issn.0529-567X.2017.05.001
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Woodley SJ, Lawrenson P, Boyle R, Cody JD, Mørkved S, Kernohan A, et al. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochr Datab Syst Rev. (2020) 5:CD007471. doi: 10.1002/14651858.CD007471.pub4
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Durnea CM, Khashan AS, Kenny LC, Durnea UA, Dornan JC, O’Sullivan SM, et al. What is to blame for postnatal pelvic floor dysfunction in primiparous women-Pre-pregnancy or intrapartum risk factors? Eur J Obstet Gynecol Reprod Biol. (2017) 214:36–43. doi: 10.1016/j.ejogrb.2017.04.036
PubMed Abstract | CrossRef Full Text | Google Scholar
4. Gartland D, MacArthur C, Woolhouse H, McDonald E, Brown SJ. Frequency, severity and risk factors for urinary and faecal incontinence at 4 years postpartum: a prospective cohort. BJOG. (2016) 123:1203–11. doi: 10.1111/1471-0528.13522
PubMed Abstract | CrossRef Full Text | Google Scholar
5. Wesnes SL, Hannestad Y, Rortveit G. Delivery parameters, neonatal parameters and incidence of urinary incontinence six months postpartum: a cohort study. Acta Obstet Gynecol Scand. (2017) 96:1214–22. doi: 10.1111/aogs.13183
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Tähtinen RM, Cartwright R, Tsui JF, Aaltonen RL, Aoki Y, Cárdenas JL, et al. Long-term impact of mode of delivery on stress urinary incontinence and urgency urinary incontinence: a systematic review and meta-analysis. Eur Urol. (2016) 70:148–58. doi: 10.1016/j.eururo.2016.01.037
PubMed Abstract | CrossRef Full Text | Google Scholar
7. Chen L, Chen X, Luo D, Jin M, Hu Y, Cai W. Performance of self-reported and unsupervised antenatal pelvic floor muscle training and its effects on postpartum stress urinary incontinence among Chinese women: a cohort study. J Int Med Res. (2020) 48:300060520914226. doi: 10.1177/0300060520914226
PubMed Abstract | CrossRef Full Text | Google Scholar
9. Viktrup L, Rortveit G, Lose G. Risk of stress urinary incontinence twelve years after the first pregnancy and delivery. Obstet Gynecol. (2006) 108:248–54. doi: 10.1097/01.AOG.0000226860.01127.0e
PubMed Abstract | CrossRef Full Text | Google Scholar
10. Pizzol D, Demurtas J, Celotto S, Maggi S, Smith L, Angiolelli G, et al. Urinary incontinence and quality of life: a systematic review and meta-analysis. Aging Clin Exp Res. (2021) 33:25–35. doi: 10.1007/s40520-020-01712-y
PubMed Abstract | CrossRef Full Text | Google Scholar
11. Li J, Li T, Huang S, Chen L, Cai W. Motivations, psychosocial burdens, and decision-making modes of post-partum women with stress urinary incontinence engaging in pelvic floor physical therapy: a qualitative research. Int Urogynecol J. (2023) 34:1803–13. doi: 10.1007/s00192-023-05466-9
PubMed Abstract | CrossRef Full Text | Google Scholar
12. Brennen R, Frawley HC, Martin J, Haines TP. Group-based pelvic floor muscle training for all women during pregnancy is more cost-effective than postnatal training for women with urinary incontinence: cost-effectiveness analysis of a systematic review [published correction appears in J Physiother. 2021 Jul;67(3):161]. J Physiother. (2021) 67:105–14. doi: 10.1016/j.jphys.2021.03.001
PubMed Abstract | CrossRef Full Text | Google Scholar
13. Seval MM, Koyuncu K. Current status of stem cell treatments and innovative approaches for stress urinary incontinence. Front Med. (2022) 9:1073758. doi: 10.3389/fmed.2022.1073758
PubMed Abstract | CrossRef Full Text | Google Scholar
14. Frawley H, Shelly B, Morin M, Bernard S, Bø K, Digesu GA, et al. An International Continence Society (ICS) report on the terminology for pelvic floor muscle assessment. Neurourol Urodyn. (2021) 40:1217–60. doi: 10.1002/nau.24658
PubMed Abstract | CrossRef Full Text | Google Scholar
15. Dumoulin C, Cacciari LP, Hay-Smith EJ. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochr Datab Syst Rev. (2018) 10:CD005654. doi: 10.1002/14651858.CD005654.pub4
PubMed Abstract | CrossRef Full Text | Google Scholar
17. Bo K, Frawley HC, Haylen BT, Abramov Y, Almeida FG, Berghmans B, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Int Urogynecol J. (2017) 28:191–213. doi: 10.1007/s00192-016-3123-4
PubMed Abstract | CrossRef Full Text | Google Scholar
18. Moossdorff-Steinhauser HF, Berghmans BC, Spaanderman ME, Bols EM. Urinary incontinence 6 weeks to 1 year post-partum: prevalence, experience of bother, beliefs, and help-seeking behavior. Int Urogynecol J. (2021) 32:1817–24. doi: 10.1007/s00192-020-04644-3
PubMed Abstract | CrossRef Full Text | Google Scholar
19. Latorre GF, de Fraga R, Seleme MR, Mueller CV, Berghmans B. An ideal e-health system for pelvic floor muscle training adherence: systematic review. Neurourol Urodyn. (2019) 38:63–80. doi: 10.1002/nau.23835
PubMed Abstract | CrossRef Full Text | Google Scholar
20. Litscher G. Integrative laser medicine and high-tech acupuncture at the medical University of Graz, Austria, Europe. Evid Based Compt Alternat Med. (2012) 2012:103109. doi: 10.1155/2012/103109
PubMed Abstract | CrossRef Full Text | Google Scholar
21. Bäumler P, Zhang W, Stübinger T, Irnich D. Acupuncture-related adverse events: systematic review and meta-analyses of prospective clinical studies. BMJ Open. (2021) 11:e045961. doi: 10.1136/bmjopen-2020-045961
PubMed Abstract | CrossRef Full Text | Google Scholar
22. Wang Q, Li N, Li J, He Y, Li Y, Zhong D, et al. A protocol of a guideline to establish the evidence ecosystem of acupuncture. Front Med. (2022) 8:711197. doi: 10.3389/fmed.2021.711197
PubMed Abstract | CrossRef Full Text | Google Scholar
23. Tang X, Shi X, Zhao H, Lu L, Chen Z, Feng Y, et al. Characteristics and quality of clinical practice guidelines addressing acupuncture interventions: a systematic survey of 133 guidelines and 433 acupuncture recommendations. BMJ Open. (2022) 12:e058834. doi: 10.1136/bmjopen-2021-058834
PubMed Abstract | CrossRef Full Text | Google Scholar
24. Liu YX. Effect of acupuncture combined with pelvic floor rehabilitation treatment on patients with postpartum stress urinary incontinence. Chin Foreign Med Res. (2022) 20:162–5. doi: 10.14033/j.cnki.cfmr.2022.05.046
CrossRef Full Text | Google Scholar
25. Tang K, Su T, Fu L, Chen Z, Liu G, Hou W, et al. Effect of electroacupuncture added to pelvic floor muscle training in women with stress urinary incontinence: a randomized clinical trial. Eur Urol Focus. (2023) 9:352–60. doi: 10.1016/j.euf.2022.10.005
PubMed Abstract | CrossRef Full Text | Google Scholar
26. Zhu LW, Zhang JY, Li J. Efficacy observation of acupuncture combined with pelvic floor muscle exercise for early-stage postpartum stress urinary incontinence. Shanghai J Acupunct Moxibustion. (2020) 39:840–3. doi: 10.13460/j.issn.1005-0957.2020.13.1019
CrossRef Full Text | Google Scholar
27. Sun Y, Liu Y, Chen H, Yan Y, Liu Z. Electroacupuncture for stress-predominant mixed urinary incontinence: a protocol for a three-armed randomised controlled trial. BMJ Open. (2021) 11:e038452. doi: 10.1136/bmjopen-2020-038452
PubMed Abstract | CrossRef Full Text | Google Scholar
28. Wang LL, Ren ZX, Zhu JY, Wu YR. Efficacy of electroacupuncture combined with penetrating moxibustion for postpartum stress urinary incontinence. Chin Acupunct Moxibustion (2019) 39:599–603. doi: 10.13703/j.0255-2930.2019.06.008
PubMed Abstract | CrossRef Full Text | Google Scholar
29. Zhang C, Luo RX, Xi JB, Liu D. Acupuncture combined with pelvic floor muscle training in the treatment of postpartum stress urinary incontinence: a meta analysis. J Pract Tradit Chin Intern Med. (2022) 36:72–5. doi: 10.13729/j.issn.1671-7813.Z20211764
CrossRef Full Text | Google Scholar
30. Shamseer L, Moher D, Clarke M, Ghersi D, Whitlock E. Preferred reporting items for systematic review and meta-analysis protocols (PRISMAP) 2015: elaboration and explanation. BMJ Clin Res. (2015) 350:g7647. doi: 10.1136/bmj.g7647
PubMed Abstract | CrossRef Full Text | Google Scholar
33. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
PubMed Abstract | CrossRef Full Text | Google Scholar
35. Liu ZY. The role of pelvic floor muscle rehabilitation training combined with psychological intervention in the nursing of postpartum stress urinary incontinence. Xin Li Yue Kan. (2022) 17:80–2. doi: 10.19738/j.cnki.psy.2022.04.027
CrossRef Full Text | Google Scholar
36. Zheng BT, Zhang GC, Zhou XH, Feng QF. Effects of acupuncture and moxibustion combined with pelvic floor rehabilitation therapy on serum relaxin, urinary fluid dynamics and quality of life in patients with stress urinary incontinence (kidney-qi deficiency type). Chin J Gerontol. (2022) 42:70–4.
Google Scholar
37. Li C, Yang M, Qu Z, Ruan S, Chen B, Ran J, et al. Effect of electroacupuncture on the degradation of collagen in pelvic floor supporting tissue of stress urinary incontinence rats. Int Urogynecol J. (2022) 33:2233–40. doi: 10.1007/s00192-022-05106-8
PubMed Abstract | CrossRef Full Text | Google Scholar
38. Li C, Qu Z, Liu J, Ruan S, Chen B, Ran J, et al. Effect of electroacupuncture on the intestinal microflora in rats with stress urinary incontinence. Front Endocrinol. (2022) 13:860100. doi: 10.3389/fendo.2022.860100
PubMed Abstract | CrossRef Full Text | Google Scholar
39. Fine P, Burgio K, Borello-France D, Richter H, Whitehead W, Weber A, et al. Teaching and practicing of pelvic floor muscle exercises in primiparous women during pregnancy and the postpartum period. Am J Obstet Gynecol. (2007) 197:107.e1–5. doi: 10.1016/j.ajog.2007.02.052
PubMed Abstract | CrossRef Full Text | Google Scholar

