Introduction
Yoga and naturopathy is one of the official indigenous systems of medicine in India under the Ministry of Ayurveda, Yoga and Naturopathy, Unani, Siddha, Sowa-Rigpa, and Homoeopathy (AYUSH), Government of India (1). Yoga and naturopathy is widely used as a lifestyle medicine for almost all systemic disorders, like musculoskeletal disorders, metabolic disorders, autoimmune disorders, neurological disorders, skin disorders, cardiovascular disorders, and respiratory disorders (2–4). Yoga and naturopathy use a holistic, patient-centered approach to treating various conditions. Hydrotherapy, therapeutic fasting, diet therapy, yoga therapy, mud therapy, heliotherapy, chromotherapy, magnetotherapy, physiotherapy, ozone therapy, acupressure, and acupuncture are the commonly used therapeutic modalities in yoga and naturopathic medicine (5). These therapies are used in combination with varying frequency as per the needs or underlying conditions of the patients. As discussed earlier, yoga and naturopathy physicians treat an array of clinical conditions, including polyneuropathies (PN), a generalized disorder of the peripheral nervous system. In our practice, we encounter PN as a comorbid condition, usually presenting along with another systemic disorder, most commonly type 2 diabetes mellitus.
Yoga and naturopathy approach in PN
India is one of the few countries in the world that operates stand-alone, state-regulated inpatient hospitals and medical colleges offering yoga and naturopathy interventions. In India, yoga and naturopathy is practiced as a holistic medical system following the international guidelines of naturopathic medicine such as: The Healing Power of Nature (Vis Medicatrix Naturae), Identify and Treat the Causes (Tolle Causam), First Do No Harm (Primum Non Nocere), Doctor As Teacher (Docere), Treat the Whole Person (Tolle Totum), and Prevention (Preventare) (6). The clinical presentation of PP can be classified into four major categories: (1) sensory symptoms (pain, loss of sensation, burning sensation, and ulcers); (2) motor symptoms (gait instability, muscle cramps, and paresis); (3) autonomic symptoms (digestive disturbances, urogenital symptoms, bladder dysfunction, tachycardia, blood pressure changes, and dryness in the skin); and (4) psychological symptoms (stress, quality of life disturbances, and sleep disturbances).
Yoga and naturopathy physicians follow a three-pronged approach in the management of all diseases, including PN, where they classify their treatments into eliminative therapies, conservative therapies, and sustainable therapies. Eliminative therapies stand for those treatments that are meant to promote elimination in the major eliminative organs like the lungs, intestine, skin, and kidney, as well as the mind, aimed at addressing the root cause, whereas conservative therapies attempt to offer symptomatic care, and lastly, sustainable therapies intend to build salutogenic health resources by offering permanent lifestyle measures (6–9). Supplementary Table S1 provides an exhaustive list of the therapies employed by yoga and naturopathy physicians in Indian settings to treat PN.
Scientific basis of yoga and naturopathic interventions for PN
Even though the evidence base literature suggesting the scientific rationale and clinical utility of yoga and naturopathic modalities is increasing over the past years, studies drawing direct inferences on the usefulness of yoga and naturopathy interventions are scarce. Hydrotherapy integrated with massage has been shown to improve the nerve growth factor, postural stability, and blood sugar levels in patients with diabetic neuropathy (10). Contrast baths have been shown to reduce neuropathic pain among patients with diabetic neuropathy (11, 12). Secondary literature suggests that hydrotherapy modalities like cryotherapy, packs, steam bath, sauna bath, head-out immersion, sitz bath, and enema to be useful in the management of various clinical conditions including PN (13, 14).
Mud therapy is another popular prescription in the management of PN. Thermal mud baths have been shown to improve the quality of life and clinical symptoms associated with diabetic polyneuropathy (15). A recent case report reported the beneficial effect of the combined yoga and naturopathy protocol in alleviating pain and improving quality of life among PN patients (16). Mooventhan et al., in their comprehensive review investigating the neuroprotective effect of yoga, have highlighted several beneficial effects of yoga in alleviating pain and improving the nerve conduction velocity in PN (17–20). Jinny et al. demonstrated that yoga therapy improves postural stability and balance in patients with PN (21). Besides this, other mind-body interventions like Reiki and meditation practices have also been shown to reduce neurotoxicity and improve the quality of life among patients with chemotherapy-induced peripheral neuropathy (22).
Fasting therapy, another commonly used modality in yoga and naturopathic practice, is also demonstrated to improve nerve function and associated symptoms by attenuating the oxidative stress and underlying metabolic disarrays in PN (23–25). Diet therapy plays a major role in yoga and naturopathic medicine-based regimens for all diseases, including PN. Plant-based diets have been shown to improve glycemic control, reduce tissue hypoxia, improve endoneurial microvasculature perfusion, and alleviate pain in patients with PN (26). Recent studies investigating the role of acupuncture in improving the clinical outcomes of PN have shown acupuncture to improve sensory and motor nerve conduction and also reduce neuropathic symptoms. Acupuncture modulates nerve growth factor signaling, attenuates inflammation, and other factors like G-protein-coupled receptor 78, purinoceptors, etc. that are associated with symptoms of PN (27, 28). Similar reports are available demonstrating the possible use of acupressure in the management of PN, especially chemotherapy-induced neuropathy and diabetic neuropathy (29, 30).
Indirect evidence indicates sun exposure (heliotherapy) to be a potential tool in modulating the cardiometabolic dysfunction that is postulated to be a risk factor for PN (31). However, there is no direct evidence available to suggest the usefulness of sun exposure, even though there are studies linking the lack of vitamin D in PN (32), for which sun exposure is a primary source. Physiotherapy treatments like exercise therapy and electrotherapy are used as an integral component of yoga and naturopathy protocols for PN. This is commonly indicated to treat the pain, muscle weakness, balance impairment and postural dysfunctions (33). Evidence suggests physiotherapy reduces the symptoms and improves the quality of life among patients with chemotherapy-induced peripheral neuropathy and diabetic polyneuropathy (33–35).
Ozone therapy, the use of ozone molecules generated from medical-grade oxygen in varying doses and forms is a well-known anti-oxidant, antibiotic, and analgesics agent (36). Numerous studies suggests the usefulness of ozone therapy in modulating the pain sensation, improving nerve conduction and reduce the symptoms associated PN (37, 38). Apart from this, a recent systemic scoping review of the treatment options for Chemotherapy-Induced Peripheral neuropathy identified numerous supportive therapies like aromatherapy, hydrotherapy, diet therapy, massage, acupuncture, acupressure, yoga therapy, and herbal medicine to have moderate to high clinical efficacy (39). Figure 1 summarizes the possible mechanisms by which yoga and naturopathic medicine therapies may attenuate the symptoms associated with PN.
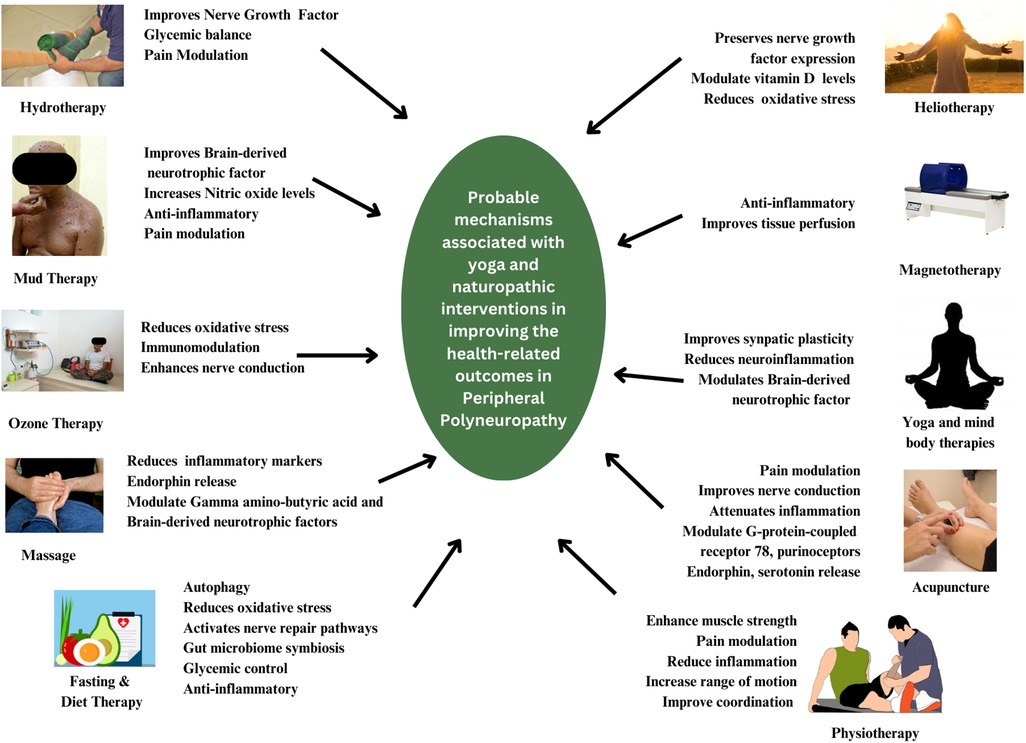
Figure 1. Yoga and naturopathy therapies’ potential biological pathways of action in polyneuropathy.
Future directions for clinical practice and research
Yoga and naturopathic medicine in India is an evidence-based practice that include a conglomerate of therapies that are drugless and holistic in nature (5). However, direct evidence demonstrating the usefulness of yoga and naturopathic medicine, as practiced in India, in the management of PN is not available in the published literature. While the user base of yoga and naturopathy is growing in India, the lack of scientific literature in PN from Indian settings depicts a serious issue of underreporting, a lack of knowledge in research and publication procedures, and a lack of motivation from public enterprises to promote research in yoga and naturopathy. Besides, some therapies used in yoga and naturopathy for PN, like chromotherapy and magnetotherapy, are solely based on anecdotal experiences or non-peer-reviewed textbook knowledge. While these therapies have shown good clinical potential, a lack of documentation harms their scientific appeal and their effective use among all stakeholders.
As discussed, yoga and naturopathy physicians in India utilize a broad range of treatment choices to manage PN. However, the choice and utility of these therapies are primarily dependent on the individual physician’s expertise, which is based on their personal experience and knowledge. There is a need to improve reporting practices among yoga and naturopathy physicians by offering high-quality training programs that would enable them to engage in evidence-based clinical practice. Given the disparities in practice patterns among Indian yoga and naturopathy physicians in the management of PN, expert committees or consensus groups that can pragmatically document clinical practices and recommend consensus guidelines to strengthen clinical practice and research are needed. Nevertheless, the present evidence hints at yoga and naturopathic medicine approaches as promising tool in the management of PN.
Author contributions
PN: Conceptualization, Data curation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. KS: Conceptualization, Methodology, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing. JK: Conceptualization, Methodology, Writing – review & editing. SK: Conceptualization, Writing – review & editing. VK: Conceptualization, Methodology, Writing – review & editing. AM: Conceptualization, Resources, Writing – review & editing. MS: Conceptualization, Resources, Writing – review & editing. NJ: Methodology, Resources, Writing – review & editing. VR: Conceptualization, Resources, Writing – review & editing. CS: Conceptualization, Resources, Writing – review & editing. KB: Conceptualization, Writing – review & editing. RM: Conceptualization, Methodology, Writing – review & editing. JS: Conceptualization, Resources, Writing – review & editing. RG: Conceptualization, Methodology, Writing – review & editing. HS: Conceptualization, Methodology, Writing – review & editing. GT: Conceptualization, Methodology, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpain.2023.1264450/full#supplementary-material
References
2. Maheshkumar K, Venugopal V, Poonguzhali S, Mangaiarkarasi N, Venkateswaran ST, Manavalan N. Trends in the use of yoga and naturopathy based lifestyle clinics for the management of non-communicable diseases (NCDs) in Tamilnadu, South India. Clin Epidemiol Glob Heal. (2020) 8(2):647–51. doi: 10.1016/j.cegh.2019.09.013
CrossRef Full Text | Google Scholar
3. Salwa H, Nair PMK. Raising burden of non-communicable diseases: importance of integrating yoga and naturopathy at primary care level. J Complement Integr Med. (2020) 18(2):271–8. doi: 10.1515/jcim-2017-0019
PubMed Abstract | CrossRef Full Text | Google Scholar
4. Nair PMK, Kriplani S, Kodali PB, Maheshwari A, Bhalavat KD, Singh D, et al. Characteristics of patients who use yoga for pain management in Indian yoga and naturopathy settings: a retrospective review of electronic medical records. Front Pain Res (Lausanne). (2023) 4:1185280. doi: 10.3389/fpain.2023.1185280
PubMed Abstract | CrossRef Full Text | Google Scholar
5. Nair PMK, Nanda A. Naturopathic medicine in India. Focus Altern Complement Ther. (2014) 19(3):140–7. doi: 10.1111/fct.12125
CrossRef Full Text | Google Scholar
7. Zeff J, Snider P, Myers S. Hierarchy of healing: the therapeutic order. The unifying theory of naturopathic medicine. In: Pizzorno JE, Murray MT, editors. Textbook of natural medicine. 4th ed. Missouri: Elsevier (2006).
10. Shourabi P, Bagheri R, Ashtary-Larky D, Wong A, Motevalli MS, Hedayati A, et al. Effects of hydrotherapy with massage on serum nerve growth factor concentrations and balance in middle aged diabetic neuropathy patients. Complement Ther Clin Pract. (2020) 39:101141. doi: 10.1016/J.CTCP.2020.101141
PubMed Abstract | CrossRef Full Text | Google Scholar
12. Gayathri M D, Nirmala T. A quasi experimental study to evaluate the effect of contrast bath therapy on neuropathic pain among diabetic patients at a selected hospital. J Diabetes Metab Disord. (2022) 9:41. doi: 10.24966/DMD-201X/100041
CrossRef Full Text | Google Scholar
13. Chaurasia G, Patil A, Dighe S. A review on therapeutic aspects of hydrotherapy. Int J Pharm Sci Res. (2015) 14(7):2713–22. doi: 10.13040/IJPSR.0975-8232.6(7).2713-22
CrossRef Full Text | Google Scholar
15. Grozeva AS, Stoycheva MI. Thalassotherapy in diabetic polyneuropathy: a study in Pomorie, Bulgaria. J Jpn Soc Balneol Climatol Phys Med. (2014) 77(5):530. doi: 10.11390/ONKI.77.530
CrossRef Full Text | Google Scholar
16. Singh P. Integrated management of diabetic peripheral neuropathy with naturopathy, yoga and diet control: a case report. Int Res J Ayurveda Yoga. (2022) 5(5):40–6. doi: 10.47223/IRJAY.2022.5507
CrossRef Full Text | Google Scholar
17. Jung M, Rein N, Fuchs B. Physical therapy for chemotherapy-induced peripheral neuropathy in pediatric oncology. Klin Padiatr. (2016) 228(6–07):313–8. doi: 10.1055/S-0042-111692
PubMed Abstract | CrossRef Full Text | Google Scholar
18. Jyotsna VP, Dhawan A, Sreenivas V, Deepak KK, Singla R. Completion report: effect of comprehensive yogic breathing program on type 2 diabetes: a randomized control trial. Indian J Endocrinol Metab. (2014) 18(4):582. doi: 10.4103/2230-8210.137499
PubMed Abstract | CrossRef Full Text | Google Scholar
21. Kanjirathingal J, Mullerpatan R, Nehete G, Raghuram N. Effect of yogasana intervention on standing balance performance among people with diabetic peripheral neuropathy: a pilot study. Int J Yoga. (2021) 14(1):60. doi: 10.4103/IJOY.IJOY_75_20
PubMed Abstract | CrossRef Full Text | Google Scholar
22. Clark PG, Cortese-Jimenez G, Cohen E. Effects of reiki, yoga, or meditation on the physical and psychological symptoms of chemotherapy-induced peripheral neuropathy: a randomized pilot study. J Evid Based Complement Altern Med. (2012) 17(3):161–71. doi: 10.1177/2156587212450175/ASSET/IMAGES/LARGE/10.1177_2156587212450175-FIG1.JPEG
CrossRef Full Text | Google Scholar
23. Kender Z, von Rauchhaupt E, Schwarz D, Tsilingiris D, Schimpfle L, Bartl H, et al. Six-month periodic fasting does not affect somatosensory nerve function in type 2 diabetes patients. Front Endocrinol (Lausanne). (2023) 14:1143799. doi: 10.3389/fendo.2023.1143799
PubMed Abstract | CrossRef Full Text | Google Scholar
24. Dannawi M, Riachi ME, Haddad AF, El Massry M, Haddad M, Moukarzel P, et al. Influence of intermittent fasting on prediabetes-induced neuropathy: insights on a novel mechanistic pathway. Metab Open. (2022) 14:100175. doi: 10.1016/J.METOP.2022.100175
CrossRef Full Text | Google Scholar
25. Sulaj A, Kopf S, von Rauchhaupt E, Brune M, Kender Z, Bartl H, et al. Six-month periodic fasting in patients with type 2 diabetes and diabetic nephropathy: a proof-of-concept study. J Clin Endocrinol Metab. (2022) 107(8):2167–81. doi: 10.1210/clinem/dgac197
PubMed Abstract | CrossRef Full Text | Google Scholar
26. Storz MA, Küster O. Plant-based diets and diabetic neuropathy: a systematic review. Lifestyle Med. (2020) 1(1):e6. doi: 10.1002/LIM2.6
CrossRef Full Text | Google Scholar
27. Dimitrova A, Murchison C, Oken B. Acupuncture for the treatment of peripheral neuropathy: a systematic review and meta-analysis. J Altern Complement Med. (2017) 23(3):164. doi: 10.1089/ACM.2016.0155
PubMed Abstract | CrossRef Full Text | Google Scholar
28. Cho E, Kim W. Effect of acupuncture on diabetic neuropathy: a narrative review. Int J Mol Sci. (2021) 22(16):8575. doi: 10.3390/IJMS22168575
CrossRef Full Text | Google Scholar
29. Yeh CH, Lukkahatai N, Campbell C, Sair H, Zhang F, Mensah S, et al. Preliminary effectiveness of auricular point acupressure on chemotherapy-induced neuropathy: part 1 self-reported outcomes. Pain Manag Nurs. (2019) 20(6):614–22. doi: 10.1016/J.PMN.2019.04.005
PubMed Abstract | CrossRef Full Text | Google Scholar
30. Yao YH, Zhang H, Li J, Zhang JP, Sun XY. Effect of modified huangqi biejiatang combined with auricular acupressure on diabetic peripheral neuropathy of qi-yin deficiency syndrome and serum MyD88/IκB signaling pathway. Chin J Exp Tradit Med Formulae. (2021) 27(11):98–105. doi: 10.13422/J.CNKI.SYFJX.20211195
CrossRef Full Text | Google Scholar
31. Fleury N, Geldenhuys S, Gorman S. Sun exposure and its effects on human health: mechanisms through which sun exposure could reduce the risk of developing obesity and cardiometabolic dysfunction. Int J Environ Res Public Health. (2016) 13(10):999. doi: 10.3390/IJERPH13100999
CrossRef Full Text | Google Scholar
32. Assy MH, Draz NA, Fathy SE, Hamed MG. Impact of vitamin D level in diabetic people with peripheral neuropathy. Egypt J Neurol Psychiatry Neurosurg. (2021) 57(1):1–7. doi: 10.1186/S41983-021-00370-9/TABLES/6
CrossRef Full Text | Google Scholar
33. Jahantigh Akbari N, Hosseinifar M, Naimi SS, Mikaili S, Rahbar S. The efficacy of physiotherapy interventions in mitigating the symptoms and complications of diabetic peripheral neuropathy: a systematic review. J Diabetes Metab Disord. (2020) 19(2):1995. doi: 10.1007/S40200-020-00652-8
PubMed Abstract | CrossRef Full Text | Google Scholar
34. Seth NH, Qureshi I. Effectiveness of physiotherapy interventions on improving quality of life, total neuropathy score, strength and reducing pain in cancer survivors suffering from chemotherapy-induced peripheral neuropathy – a systematic review. Acta Oncol. (2023) 62(9):1143–51. doi: 10.1080/0284186X.2023.2238890
PubMed Abstract | CrossRef Full Text | Google Scholar
35. Andersen Hammond E, Pitz M, Steinfeld K, Lambert P, Shay B. An exploratory randomized trial of physical therapy for the treatment of chemotherapy-induced peripheral neuropathy. Neurorehabil Neural Repair. (2020) 34(3):235–46. doi: 10.1177/1545968319899918/ASSET/IMAGES/LARGE/10.1177_1545968319899918-FIG3.JPEG
PubMed Abstract | CrossRef Full Text | Google Scholar
36. Viebahn-Hänsler R, León Fernández OS, Fahmy Z. Ozone in medicine: the low-dose ozone concept—guidelines and treatment strategies. J Int Ozone Assoc. (2012) 34(6):408–24. doi: 10.1080/01919512.2012.717847
CrossRef Full Text | Google Scholar
37. Clavo B, Martínez-Sánchez G, Rodríguez-Esparragón F, Rodríguez-Abreu D, Galván S, Aguiar-Bujanda D, et al. Modulation by ozone therapy of oxidative stress in chemotherapy-induced peripheral neuropathy: the background for a randomized clinical trial. Int J Mol Sci. (2021) 22(6):1–19. doi: 10.3390/IJMS22062802
CrossRef Full Text | Google Scholar
38. Bruno AS. Oxygen-ozone and α-lipoic acid in the treatment of peripheral neuropathies conflicting therapies or synergistic association? Ozone Ther. (2018) 3(1):1–3. doi: 10.4081/ozone.2018.7517
CrossRef Full Text | Google Scholar
39. Klafke N, Bossert J, Kröger B, Neuberger P, Heyder U, Layer M, et al. Prevention and treatment of chemotherapy-induced peripheral neuropathy (CIPN) with non-pharmacological interventions: clinical recommendations from a systematic scoping review and an expert consensus process. Med Sci (Basel). (2023) 11(1):15. doi: 10.3390/medsci11010015
PubMed Abstract | CrossRef Full Text | Google Scholar

