Search and selection
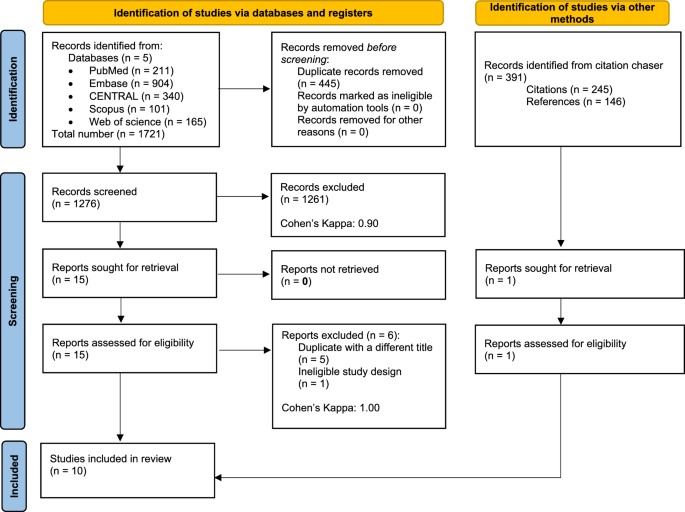
A total of 1,721 records were identified in five databases, including 904 in Embase, 211 in MEDLINE (via PubMed), and 340 in CENTRAL., 101 in Scopus and 165 in Web on Science. After removing duplicates, 1,276 records remained for title and abstract selection.A total of 15 studies were assessed for full text eligibility, of which 6 were excluded38,39,40,41,42,43.Five of the six excluded studies were duplicates but had different titles38,40,41,42,43one had an ineligible study design39. Furthermore, although he identified 391 records through citation tracking, only one of his studies was retrieved for the search and included in the data extraction.44. See the PRISMA flowchart (Figure 1) for details on the search and selection process.
Flowchart of the PRISMA article selection process.
Basic characteristics of included studies
Our study consisted of 10 RCTs with a total of 1,051 patients.5,7,13,14,15,16,44,45,46,47.One of these studies was presented as a conference abstract47. Five of the 10 studies focused on patients with non-variceal upper gastrointestinal bleeding (NVUGIB), primarily PUB.13,16,45,46,47and the other five focused on VUGIB patients.5, 7, 14, 15, 44. The study was conducted in different geographic locations: five in Asia, three in Europe, one in Africa, and one in North America. See (Table 1) for study details including basic characteristics.
Early rebleeding (within 7 days)
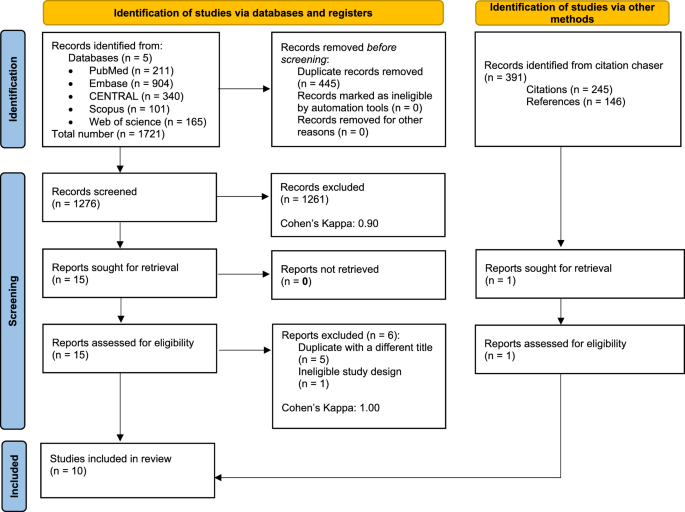
We analyzed 8 trials5, 7, 13, 14, 15, 16, 44, 45 The study included 923 patients (465 in the EN group and 458 in the DN group) who reported rebleeding within 7 days. In the VUGIB subgroup, our analysis showed no significant difference between the two groups (RR 1.48, 95% CI 0.38 to 5.71). The same was true for the PUB subgroup (RR 0.95, 95% CI 0.54 to 1.68). Overall, EN did not significantly or associatedly increase the risk of early rebleeding compared with DN (RR 1.04, 95% CI 0.66 to 1.63; p = 0.845, I2 = 0%, 95% CI 0 to 68%) (Figure 2).
Forest plot showing the effect of early versus delayed nutrition on early rebleeding (within 7 days) after upper gastrointestinal bleeding. RR risk ratio, CI Confidence interval.
Late rebleeding (within 30-42 days)
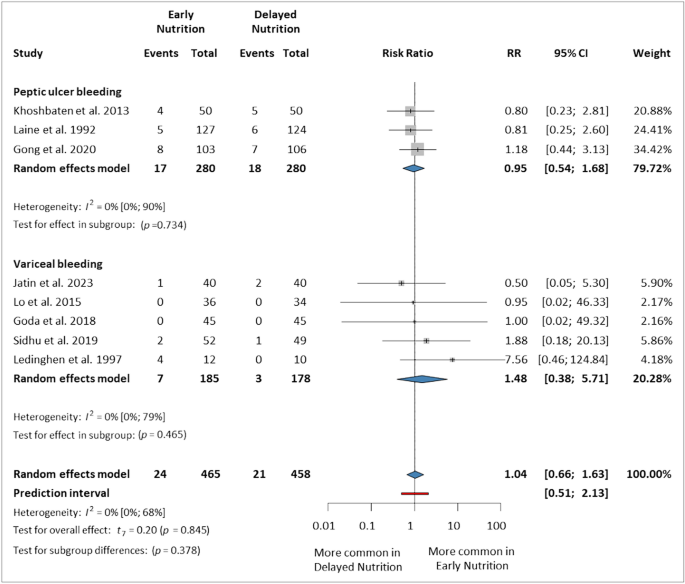
Eight studies were included in this analysis5,7,14,15,16,44,46,47 The study included 693 patients (347 in the EN group and 346 in the DN group) who reported rebleeding within 30, 35, or 42 days. The results were not statistically significant in either subgroup including PUB (RR 1.14, 95% CI 0.16-7.98) and VUGIB (RR 1.13, 95% CI 0.40-3.17). Overall, EN did not increase the risk of late rebleeding compared with DN (RR 1.16, 95% CI 0.63 to 2.13, p = 0.583, I2 = 0%, 95% CI 0 to 68%) (Figure 3).
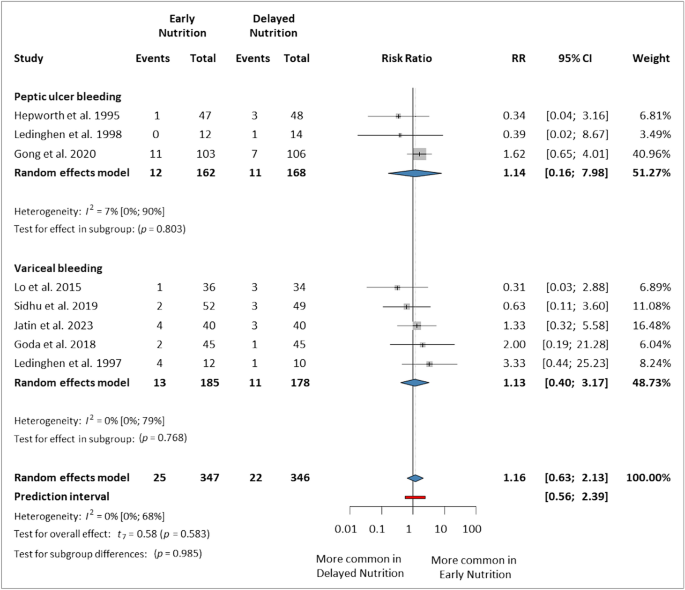
Forest plot showing the effect of early versus late nutrition on late rebleeding (within 30-42 days) after upper gastrointestinal bleeding. RR risk ratio, CI Confidence interval.
Early mortality (within 7 days)
just 5 studies7,13,15,44,45 Patients who reported mortality within 7 days were included in this analysis, resulting in a total of 543 patients (234 in the EN group and 229 in the DN group). There were no statistically significant differences between studies in the PUB and VUGIB subgroups (RR 0.98, 95% CI 0.85 to 1.14 and RR 1.36, 95% CI 0.63 to 2.91, respectively). The overall effect was not statistically significant between the two groups (RR 1.20, 95% CI 0.85 to 1.71, p = 0.214, I2 = 0%, 95% CI 0 to 79%) (Figure 4).
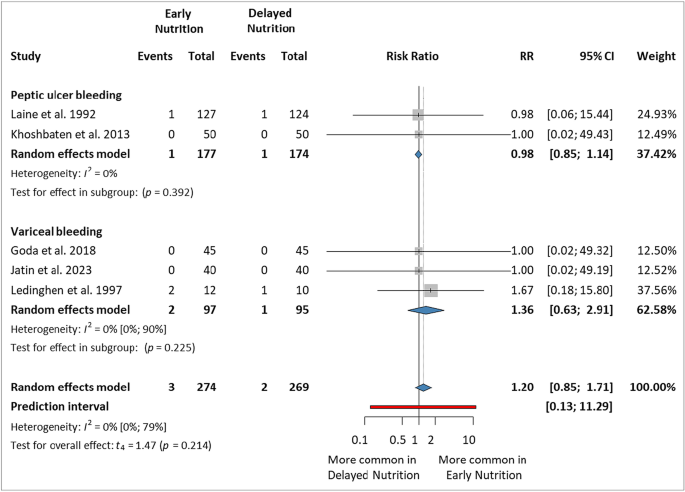
Forest plot showing the effect of early versus delayed nutrition on early mortality (within 7 days) after upper gastrointestinal bleeding. RR risk ratio, CI Confidence interval.
Late mortality (within 30-42 days)
Seven studies were included in the analysis5, 7, 14, 15, 16, 44, 47 Death reported within 30, 35, or 42 days. A total of 667 patients participated (335 in EN group, 332 in DN group). There were no statistical differences in either subgroup. PUB subgroup (RR 0.51, 95% CI 0.03 to 7.83) and VUGIB subgroup (RR 0.73, 95% CI 0.26 to 2.02). Overall, there was no statistically significant difference between the two groups. However, the results were clinically relevant, with a trend in the EN group (RR 0.61, 95% CI 0.35 to 1.06; p = 0.072, I2 = 0%, 95% CI 0 to 71%) (Figure 5).
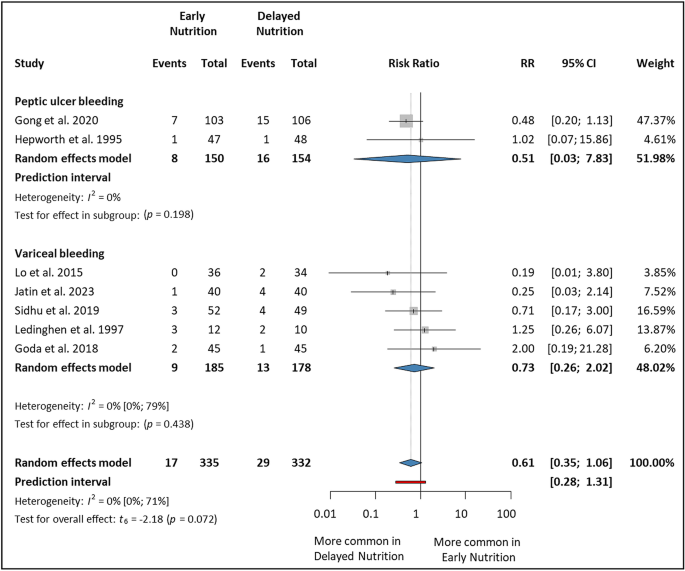
Forest plot showing the effect of early versus delayed nutrition on late mortality (within 30-42 days) after upper gastrointestinal hemorrhage. RR risk ratio, CI Confidence interval.
Hospitalization period (days)
This analysis included 6 studies5, 7, 13, 14, 45, 46 A total of 570 patients participated (289 in the EN group and 281 in the DN group). In the PUB subgroup, there was no statistically significant difference between the two groups (MD: -1.34 days, 95% CI -5.01 to 2.33), but in the VUGIB subgroup, EN significantly reduced LOS. (MD: -1.54 days, 95% CI) -2.67 to -0.41). Overall, EN reduced LOS compared to DN (MD −1.22 days, 95% CI −2.43 to −0.01; p= 0.049, I2 = 94%, 95% CI 90–97%) (Figure 6).
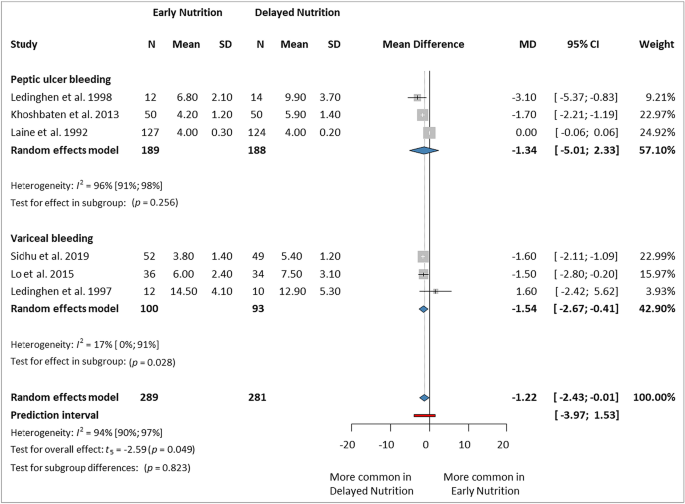
Forest plot showing the effect of early versus delayed nutrition on length of hospital stay after upper gastrointestinal bleeding. Nnumber of patients in each arm, SDstandard deviation, medical doctormean difference, CIConfidence interval.
Jatin et al.15and Gong et al.16 We reported results as medians rather than means. We decided to exclude these studies from the final analysis due to the possibility of biasing the results. However, even when estimating the mean from the median provided, the results show a significant reduction in LOS (MD -1.12 days, 95% CI -2.03 to -0.22, p= 0.022, I2 = 93%, 95% CI 88–96%) (Supplementary material Fig. S1).
Blood transfusion requirement (unit)
7 studies5, 7, 13, 14, 16, 45, 46 As a result, the need for blood transfusion was reported. However, he was only able to analyze 4 studies (292 in the EN group and 286 in the DN group).5, 16, 45, 46This is because the definition of this outcome differs between the included studies (summarized in Supplementary Material Table S3). Overall, there was no statistically significant difference between the two groups (MD 0.00, 95% CI -0.04 to 0.05; p= 0.980, I2 = 0%, 95% CI 0 to 85%). (Supplementary Material Figure S2).
Bacterial infection
only 3 studies5, 14, 15New-onset bacterial infections were reported, including 251 patients (128 in the EN group and 123 in the DN group). Overall, there was no statistically significant difference between the two groups (RR 0.48, 95% CI 0.08 to 3.05; p= 0.229, I2= 0%, 95% CI 0–90%) (Supplementary Material Figure S3).
Ascites and hepatic encephalopathy
Three studies reported on new-onset ascites.5, 14, 15. Overall, ascites tended to be more common in the DN group, although this was not statistically significant (RR 0.64, 95% CI 0.34 to 1.20; p= 0.094, I2= 0%, 95% CI 0–90%) (Supplementary Material Figure S4).In addition, two studies5,15We reported on newly developed hepatic encephalopathy. (RR 1.03, 95% CI 0.50-2.11 and RR 0.75, 95% CI 0.18-3.14, respectively). Only he was unable to draw statistical inferences based on the two studies. Therefore, we presented this result in Figure S5 in the Supplementary Material without any global impact.
ICU admission rate and blood transfusion rate
No statistical conclusions could be reached regarding these results.just one study45Date of ICU admission was reported. There was no difference between the two groups (EN: 1.1 ± 0.2, DN: 1.1 ± 0.1). In one study15Reported need for ICU admission (EN: 1/40, DN: 2/40). No studies reported data on transfusion rates.
Risk of bias assessment and quality of evidence
The article said the randomization process and choice of reported outcome domains raised “some concerns.” Deviations from planned interventions and missing outcome data had the lowest risk of bias. Bias due to outcome measurement was high for outcomes of LOS and new-onset hepatic encephalopathy. The results of the risk of bias assessment by outcome for all included studies are shown in the figures in the supplementary material. S6 to S12.
The quality of evidence was low or very low for all outcomes. A summary table and description of the results can be found in the supplementary material (Supplementary Tables S4–S5).
Heterogeneity and publication bias
All analyzes of included outcomes showed negligible levels of statistical heterogeneity (I2), heterogeneity was 0% or <10% (CI 90–97%), except for the LOS outcome, which was 94%. This discrepancy may be due to variation in bleeding severity between patients, which impacts the need for hospitalization. Omitting Laine et al., we found that:study45In a leave-one-out sensitivity analysis that included patients with less severe disease compared to other studies, the effect size became more significant (MD -1.65 days, 95% CI -1.99 to -1.31), and the heterogeneity 5% (Supplementary Fig. S13–14). Regarding publication bias, the diagnostic accuracy of the test was limited to less than 10 of his studies, and none of the analyzes met this threshold, so we decided to exclude this analysis.