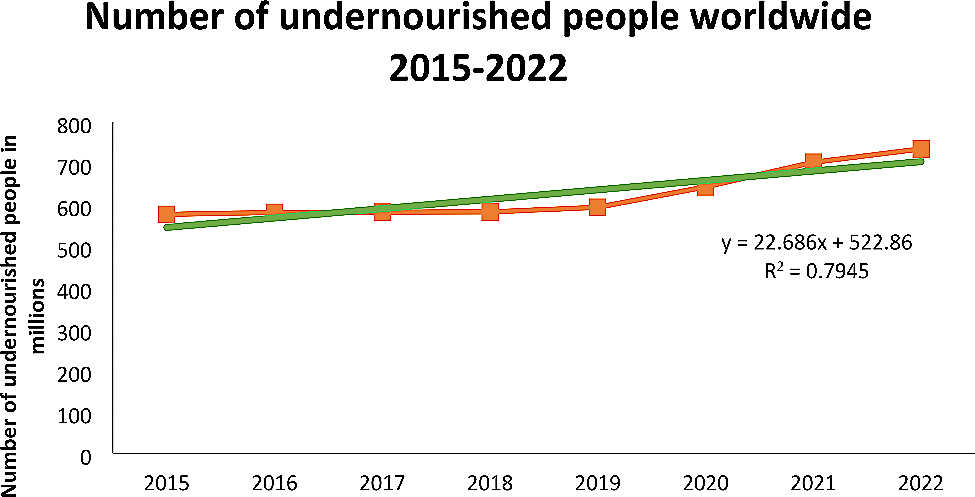
Our trend analysis shows that global hunger and undernourishment will increase over time from 2015 to 2022, contributing to tuberculosis (TB) incidence and the World Health Organization’s (WHO) end-TB goal. It has been shown to have a significant impact on achievement. According to the WHO, undernutrition has been identified as one of the most important factors for tuberculosis, accounting for an estimated 19% of tuberculosis cases worldwide in 2020. [15].Study reveals undernourished people are three times more likely to develop tuberculosis [16, 17]. Malnutrition can impair immune and vaccine responses to tuberculosis, leading to increased risk of infection, progression, and transmission. [18]. Additionally, nutritional deficiencies can worsen the severity of tuberculosis, leading to poor treatment outcomes, including increased mortality and recurrence rates. [19, 20].
Our trend analysis shows that forced evacuations are increasing over time. Addressing this problem requires a comprehensive and coordinated effort by various stakeholders, including governments, health authorities, humanitarian agencies, donors, and civil society, to achieve TB elimination goals. Forced displacement can increase the risk of tuberculosis infection among displaced populations. This is because they often live in overcrowded, unsanitary and unstable conditions. [21, 22]. This could also encourage the spread of drug-resistant strains of tuberculosis, which are harder and more expensive to treat. [23].
According to data from the World Health Organization (WHO), a study conducted among internally displaced persons (IDPs) in north-eastern Nigeria and Sudan, areas deeply affected by political conflict and insurgency, found that tuberculosis was particularly prevalent among internally displaced persons (IDPs). was found to have a negative impact on detection and treatment results. Among the refugees. The findings pinpointed key factors influencing access and utilization of TB services among internally displaced people, including safety concerns, social stigma, and lack of awareness. [24].Forced migration can impede continuity of TB services, including diagnosis, treatment, and follow-up care. [25]. Displaced people may face barriers to accessing health facilities, including distance, cost, safety, and stigma. You may also lose your medical records, medications, and contacts with health care workers during the evacuation. [26, 27]. This can lead to delayed diagnosis, interruption of treatment, poor prognosis, and increased mortality. [22].
Forced migration may therefore hinder the implementation of End TB Strategies, which require a multisectoral and people-centred approach to ending the TB epidemic. Conflict and forced migration can undermine the political commitment, financial resources, and coordination mechanisms needed to achieve strategic goals and objectives.
Our research highlights that the global burden of homelessness is increasing over time, posing major challenges to achieving the TB elimination goal by 2035. Homelessness is a major risk factor for tuberculosis, with crowded and unsanitary conditions exposing people to the tuberculosis bacteria. [28, 29].Immune stressors associated with homelessness, including disturbed sleep, malnutrition, and substance abuse, increase the likelihood of developing tuberculosis [30, 31]. Homeless people often delay seeking medical help due to misinterpretation of TB symptoms, and face barriers in accessing and adhering to TB treatment, including a lack of social support and stable housing. doing. [32, 33].
In the United States, 20,104 studies from 1994 showed that the incidence of tuberculosis was more than 10 times higher among people experiencing homelessness compared to people who did not experience homelessness. [34]. In Ethiopia, homeless people have approximately 4.67 times higher smear-positive PTB than the general population. [35].In addition, the incidence of tuberculosis in homeless people is four times higher than in the general population [36]. Additionally, diagnosing, treating, and preventing tuberculosis among homeless people is challenging. [37]. Barriers to TB control among homeless people include lack of awareness, stigma, mistrust, mobility, and competing priorities. [38, 39].
The COVID-19 pandemic has had a significant impact on global health systems, disrupting essential services and posing challenges to achieving the WHO goal of eliminating tuberculosis, according to the WHO Tuberculosis Report 2022. It can make things even worse. Although quantifying these impacts is complex, the pandemic has significantly reduced notification of tuberculosis cases and estimated increases in tuberculosis deaths during the peak years of 2020 and 2021. It is recognized that the overall figures are likely to have worsened.